24th September 2017
‘The flow of rivers and streams in their boundaries . . . the circulation of the blood in our arteries and veins . . . the flight of the insect, the bird and the airplane; the movement of a ship in the water or of a fish in the depths . . . these are all, in major degree, varied expressions of the laws of fluid mechanics … Everywhere we find fluids and solids in reactive contact, usually in relative motion; and everywhere in this domain, the laws of fluid mechanics must control.
Application of the laws of fluid mechanics to the natural conditions in the circulatory system reveals a rational and demonstrable basis for the localization, inception, and progressive development of atherosclerosis.
Atherosclerosis does not occur at random locations. It does occur uniformly at specific sites of predilection that can be precisely defined, predicted, and produced by applying the principles of fluid mechanics. The areas of predilection for atherosclerosis are consistently found to be the segmental zones of diminished lateral pressure produced by the forces generated by the flowing blood.
Such segmental zones of diminished lateral pressure are characterized by tapering, curvature, bifurcation, branching, and external attachment. Serpentine flow in a relatively straight vessel also produces segmental zones of diminished lateral pressure.
Although these anatomic configurations occur in many variations of geometry, their common feature is a pattern of blood flow conducive to the production of localized areas of diminished lateral pressure. This is the initial stimulus.
Atherosclerosis may therefore be considered to be the biologic response of blood vessels to the effect of the laws of fluid mechanics, that is, the diminished lateral pressure generated by the flowing blood at sites of predilection determined by local hydraulic specifications in the circulatory system.’1
Not my words, and quite poetic I suppose. What does it mean. It means, if you accept what is written, is that atherosclerosis forms exactly where you would expect it to form – if the initial stimulus is ‘diminished lateral pressure’.
My last blog was primarily a looking at the primary stimulus for the initial formation of atherosclerotic plaques. I like to use the term biomechanical stress. I am not entirely certain if this means anything. But the general idea is that atherosclerotic plaques start at the points in blood vessels where there is the greatest ‘biomechanical stress.’
Several people who know far more about fluid dynamics questioned this. I think that they are all probably right in what they say, and the mathematics are well beyond my understanding. However, what I do know, and what are facts, are the following:
- Atherosclerotic plaques inevitably occur where is there is tapering, curvature, bifurcation, branching and areas of external attachment.
- Plaques never develop in veins, regardless of tapering, curvature and branding and suchlike.
- Plaques never develop in the arteries and veins in your lungs – unless you develop pulmonary hypertension (raised blood pressure in the lungs) – though a caveat applies.
- Plaques often appear on one side of an artery, and not the other (i.e., they do not encircle the artery).
- If you take a vein from the leg, and use it as a coronary artery bypass graft, it will rapidly develop atherosclerotic plaques.
Therefore, whatever term you want to use, however, you wish to understand it, it is clear that in order to get a plaque to start, you need to apply some form of ‘stress’ to the blood vessel, and the blood pressure needs to be at a certain level – or else nothing will happen. This is true, no matter what the LDL level, or the blood sugar level, or whether you smoke, or [insert any one of eight thousand risk factors here].
Ergo, there must be some form of damage occurring at the point of high biomechanical stress, that triggers plaque development. Under biomechanical stress, the first part of the artery to suffer will be the endothelium – the layer of cells that lines the arteries. If endothelial cells are stressed, damaged, or dysfunctional, this is the trigger for plaques to start:
‘In view of the ever-increasing prevalence of ischaemic heart disease in the developed and developing world, it has become imperative to identify and investigate mechanisms of early, potentially reversible pre-atherosclerotic changes in the endothelium. To date, the most clearly defined and well-understood early precursor of atherosclerosis is Endothelial Dysfunction. In fact, Endothelial Dysfunction can be regarded as the primum movens of atherosclerotic disease.’2
I guess that primum movens is Latin for ‘the single most really important thing.’
In short, you damage the endothelium, and that releases the atherosclerotic dogs of war. What sort of things are known to increase endothelial stress/damage. Here is a list, off the top of my head, of a few factors that have been identified.
- Smoking
- Air pollution
- Diabetes
- Cocaine use
- Dehydration
- Infections/sepsis
- Systemic Lupus Erythematosus (SLE)
- Lead
- Stress hormones
- Avastin
- Omeprazole
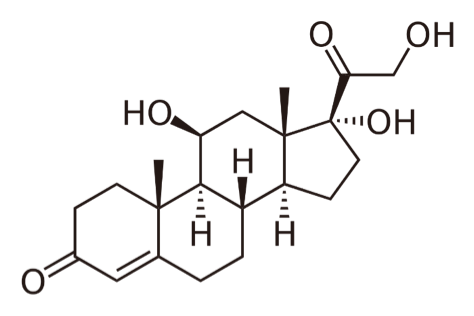
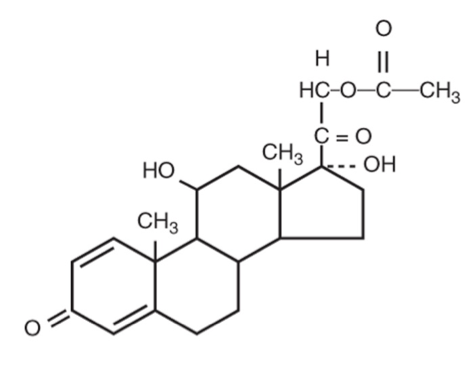
- Cushing’s disease
- Kawasaki’s disease.
I could go on, and on, but I think that is enough to be going on with. All of these factors have been demonstrated to cause significant damage to the endothelium – in different ways – and there is another thing that they all do. They all increase the risk of dying of CVD. Some of them enormously increase the risk. A young woman with SLE has an increased risk of dying of CHD of 5000% (relative risk increase).
When you are looking at a 5000% increase in risk you are, without the slightest shadow of a doubt, looking at a cause.
The only other increased risk I have ever seen to match this, or in fact beat this, is in young people with sickle cell anaemia where the increased risk of stroke is 33,000% (relative increase in risk). Yes, not many young people get strokes, but an increase of 33,000% is difficult to argue with.
Why do they get so many strokes? It is, in part, because the ‘sickle’ shaped red blood cells clump together more easily than normal shaped red blood cells. Once they clump together, they form clots, and these clots block arteries. Often in the brain – but also elsewhere. It is not as simple as this, but that will do for now.
There is another thing about sickle cells anaemia that I find of great interest. It is the only condition (at least the only condition I have come across), where atherosclerotic plaques can form in the lungs – at normal blood pressure.3
Why does this happen? Well sickle cells are not round and smooth. They are crescent shaped, and spiky at the ends, and stiffer than normal red blood cells, and they are more likely to cause mechanical damage to the endothelium.
‘A further mechanism of endothelial dysfunction is attributed to the rigidity of sickled erythrocytes (red blood cells) causing mechanical injury to the endothelial cells.’3
In addition:
‘The sickling process leads to vascular occlusion, tissue hypoxia and subsequent reperfusion injury, thus inducing inflammation and endothelial injury. This causes a blunted response to nitric oxide (NO) synthase inhibition.’3
Yes, our old friend Nitric Oxide again. Put simply, sickle cells crash into, and damage endothelial cells, which then stop producing as much NO. This endothelial dysfunction then leads on to atherosclerosis. All of this happens with no other risk factors present, and in arteries where atherosclerosis is normally never seen. Which means that we are looking very directly at cause, and effect. Physical damage to endothelial cells, no other factors required.
Now, I am aware that many people wonder why my series on what causes heart disease/cardiovascular has been so long and meandering. One major reason is that there is so much to try and find out, and explain. Also, and perhaps more critically, if you are going to try and understand cardiovascular disease fully, you must attempt to fit everything together, and that does take time.
For example, you must explain how: SLE, sickle cell anaemia, Kawasaki’s disease, omeprazole, diabetes, smoking and infections (to name but seven) can all cause CVD when, superficially, there is nothing to link them. Certainly none of the established, mainstream, risk factors.
There is no point in saying that, yes, they all cause heart disease, and that’s that, just add them to the list. There is a requirement to fit them within a single process, and it must make sense. It also has to be supported by the facts – as far as that is possible.
Equally, there is no point in saying CVD is ‘multifactorial’, which is the normal defence of the mainstream when pressed on why many people, with no risk factors for CVD, still get CVD. The word “multifactorial” explains nothing, it is just an escape route for those pressed to explain the many ‘paradoxes’ or refutations that keep on appearing.
If, for example, you cannot explain how sickle cell anaemia causes atherosclerotic plaque formation, in pulmonary arteries, this means you do not understand, or do not wish to understand, the underlying process. It fits nowhere within the accepted major risk factors, yet it increases the risk of stroke by 33,000%, and causes plaques to develop in the lungs. So, you cannot just ignore it, relatively rare though it may be.
So, where have we got to? Where we have got to, I believe is to demonstrate that the trigger factor for CVD is damage to the endothelium. If you don’t damage the endothelium nothing else happens. The damage happens at well recognised places where the biomechanical stress is at its greatest. Which means that, with no biomechanical stress, there can be no atherosclerotic plaques.
However, it takes more than just biomechanical stress. You also have to have, at least one, extra factor present to trigger endothelial dysfunction. Then … next episode.
References:
1: From Chapter 8 Coronary Heart Disease: The Dietary Sense and Nonsense: George V. Mann: 9781857560725: Amazon.com: Books