29th December 2023
The underlying forces
In the last few blogs, I have been writing about the proliferation of guidelines, targets, and regulatory work in the NHS. Hopefully I have managed to give you a sense of how much time and effort these pile on to everyday work. Time and effort which eats away at clinical time, erodes morale and drives down productivity.
None of this is unique to the NHS. It is not unique to healthcare, and it is certainly not unique to the UK. An ever-tightening regulatory framework is affecting almost everyone, worldwide. ‘Ratchet world’ as I call it.
However, I believe that healthcare, specifically the NHS, represents the highest regulatory pinnacle. The Mount Everest in the target and regulation world. This is because it is driven by three different, but interconnected forces:
- The risks attributed to medico-legal/patient harm.
- Complexity – and the desire to micromanage.
- The size of the organisation.
Medico-legal pressure to record absolutely … everything
In this blog I am only going to start looking at the first of these forces. Medico-legal/patient harm. Even here I can barely scratch the surface.
‘The provision for claims against the NHS increased from £85.2 billion ($108 Bn) to £128.6 billion ($163Bn) n March 2022.’ 1
More and more people are suing the NHS for damages. More and more people are complaining about their treatment, whether or not they go on to sue.
Is care getting worse, or does this represent a rise in complaint culture? ‘No-win no-fee’ lawyers are certainly advertising harder than ever. And if you think your care went wrong, why not sue? There’s nothing to lose, and you could end up several thousand pounds richer. Maybe far more.
Whatever the underlying reasons, complaints clog up the machine, directly and indirectly. Even if they are not ‘successful’, they take up vast amounts of time to resolve. Not that long ago I received a nasty complaint about my poor care for a patient. I was on holiday at the time and could easily prove it.
I still had to spend many, many hours dealing with it. So did my manager, and the complaints team at the hospital. And the unit manager and …One phone call by the General Medical Council was all that was needed. ‘Yes, he was on holiday all week.’
Leaving that to one side. The issue I want to look at here is the downstream, or indirect impact, that the threat of litigation creates. The moment any complaint arrives, management circle the wagons, then pore through the patient’s notes to check that all guidelines and regulations were followed – to the letter.
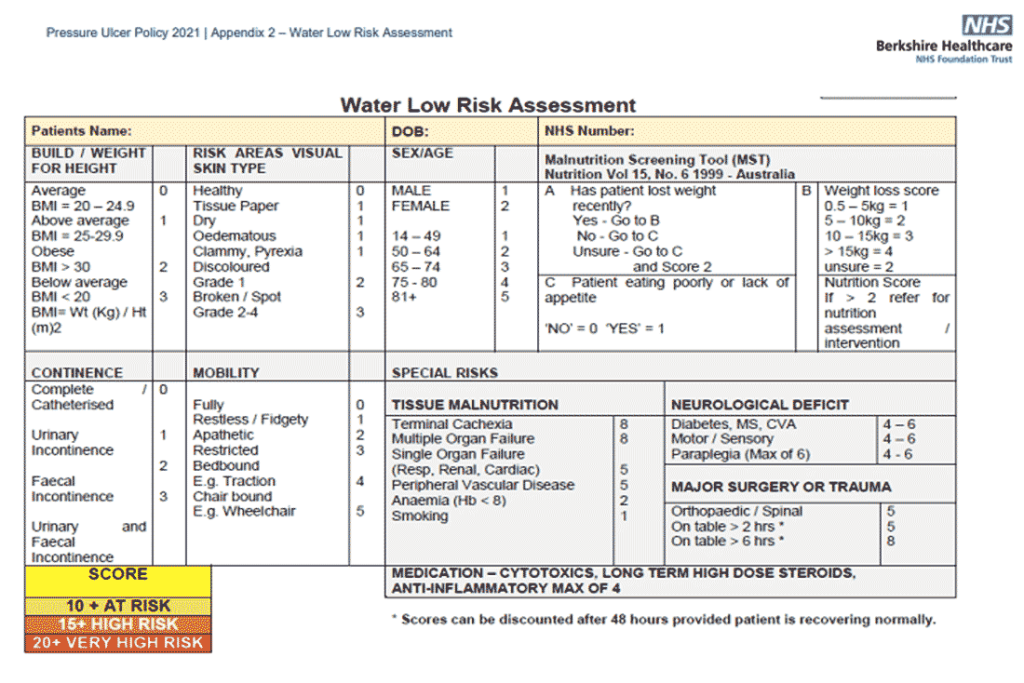
Was the falls audit done? Were all the Water Lows done? Were all care indicators filled in. Below is an example of a ‘Water Low’ chart. It has to be completed within six hours of admission, repeated if there is any change in the clinical condition, and done at least weekly otherwise, in some cases up to three times a week. God help you if it is missing.
And, no, I don’t know why it is called Water Low. I think it should actually be Waterlow.
There can’t be any gaps in ‘excellent’ patient care. All cups of tea offered, and drunk, with the correct number of sugars stirred clockwise. Everything will be scrutinised. The mantra here, as always, is that: ‘if it isn’t written down, it wasn’t done.’
Recording everything, no matter how unimportant, is how lawyers believe a perfect world should be ordered. Their view is that you cannot possibly defend yourself by saying. ‘Of course I did that, it’s what all doctors do. What we are trained to do. Now, you need to prove I didn’t. I shouldn’t need to prove I’m innocent, you need to prove I’m guilty’… Jurisprudence page one, paragraph one. In England least. [Scots law is subtly different]
When I started out in GP-land, all consultations were written out by hand, and we had seven minutes per appointment. Which included the patient’s agonisingly slow walk along the corridor, trying three wrong doors along the way, taking a history, the examination, making a diagnosis, and writing notes. Then, finishing with a prescription. Along with any friendly chat.
If someone had a cough, and possible chest infection, the entire consultation could be written up as. LRTI. Rx Amoxicillin 500mg TDS. Review 1/52 if symptoms no better. MK. 12/6/1993
[Translation: Lower respiratory tract infection. I prescribed amoxicillin 500mg three times daily. I advised the patient to come back in a week if symptoms were no better. My initials and date at the end].
This would now be considered indefensible medical practice. Why did I fail to record the respiratory rate, the oxygen levels, the blood pressure, what did I hear in the chest? Were there signs of possible sepsis, and on and on and on.
You know, if there had been anything important to find, I would have written it down. And if I believed the patient was ‘proper’ ill, I would have sent them to hospital. Or asked them to come back in the next day to make sure they were not getting worse. But no, not now. All shall be written down.
Inexorably, we have ended up with endless drivel in the notes, from all and sundry. ‘I went into the room and introduced myself as George, a physiotherapist. I checked how the patient would like to be identified. They said their name was Mabel, but they like to be called Iris. They consented to my examination ….’ And on, and on. Names changed for patient confidentiality.
In my view anyone writing nonsense like this inpatient notes should be taken to one side and told, in no uncertain terms, to stop writing this bilge … right now, immediately, and never do it again.
It is a complete and utter waste of everyone’s time. It is not clinically relevant in any way. It also makes it almost impossible to find anything that might be important buried in there somewhere. Such as, what you thought was wrong with the patient, what you actually did, and what happens next, and anything you would like me to do …George.
However, management absolutely love this exponential expansion in record keeping. Indeed, they want more, and more … and more. When a complaint comes in, they can point to this endless verbiage.
The chest was examined for fifteen minutes, all negative findings meticulously recorded. Nothing was actually found anywhere else, meticulously recorded. Although they complained of a headache, I spent ten minutes examining their abdomen, all recorded.
I do not want to know what is ‘not’ wrong with the patient. I want to know what is wrong with the patient. This nonsense comes to a head with NHS 111. This is the service that patients can call, outside of GP surgery opening times. If they are unwell, but do not need an ambulance.
NHS 111 staff record everything, every breath taken. They are especially keen on capturing information about what the patient does not have wrong with them. The patient had not suffered a head injury, the patient was not pregnant, and on, and on.
Their reports now run to nineteen pages, with a great deal of information about what the patient did not have. Sitting on the receiving end, I do not even bother to read them. Because it is almost impossible to find out why the patient called in the first place.
It will be in there somewhere. But it should be page one, line one. ‘The patient called the service because they had a bad headache.’ This may be buried on page five. After two pages recording when the patient called, who took the call, when it ended, what phone numbers were used. What service the patient was referred to, by whom, when. Sigh. Followed by another two pages of conditions that the patient does not have. The patient was NOT hit by an asteroid.
When the patient arrives in my room, having been directed to see a doctor by NHS111, I just ask. ‘What seems to be the problem today?’ They always look aghast. ‘But I have already told NHS 111 all this.’ Yes, but there is not the time in the day for me to read such endless, pointless, garbage… I think this, but do not say it. I just smile in a kind and reassuring way. Whilst snapping a pencil in two under the desk.
The function of medical records is not for them to be written in such a way that they can be used to defend against litigation. It is to pass clinically important information between medical professionals, to enable them to do their job better. Therefore, it must be brief – and to the point.
Try saying that to a manager in the NHS. It is a concept so alien to them, that they almost certainly cannot understand what you just said. Blink! Hard disk reset.
I was recently told that I should write something in the patient notes, every day. Such as what? ‘Clinically, the patient is exactly the same today as they were yesterday. So I didn’t examine them, or prescribe anything.’’ What of patients attending hospital out-patients for a review when I go to see them? ‘The patient was not in the unit today, so I do not know if they are clinically unchanged since yesterday.’
Is that the type of thing you’re looking for?
Yes, was the answer.
Can we row this back?
Perhaps we could start with Winston Churchill who, as always, puts it best.
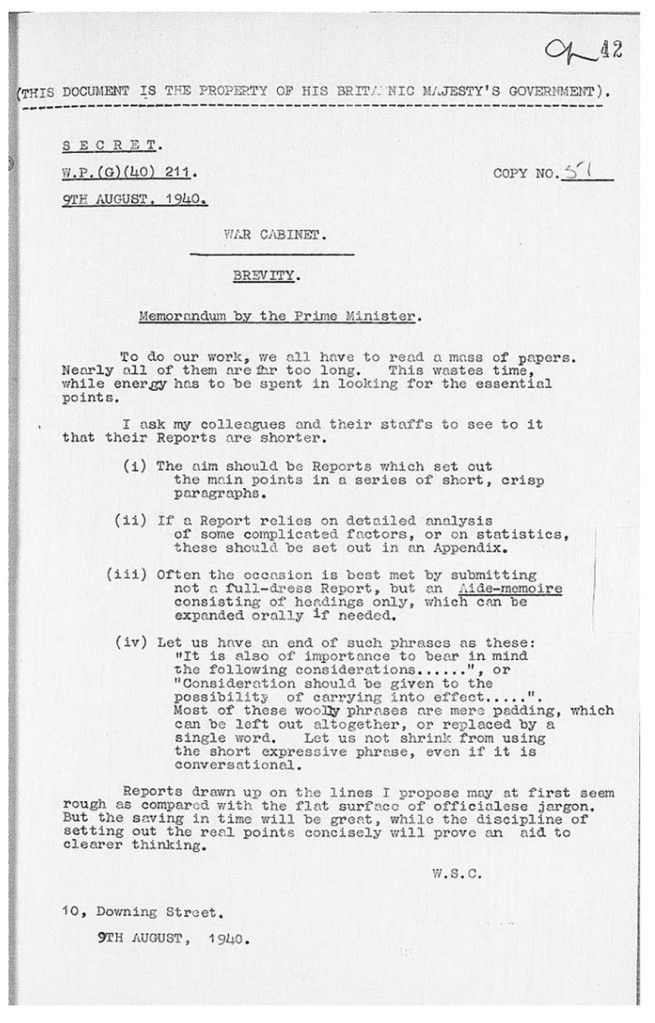
Churchill knew, as we all know, that pages of meaningless guff serve only to block effective communication. For example, the notes that arrive with patients from the local hospital are, still, written out by hand. It is literally impossible to gain any useful information.
If I do manage to raise the enthusiasm to read them, I find that I often have no idea why the patient was admitted, what happened to them, or why. But, by crikey, you need to go the gym regularly to lift them.
Brevity is what we need. But endless recording, of everything, is what we get. Along with a massive increase in the ‘everything else’ that simply must be done. It is a great burden to carry. It gets heavier every day. It is driven by a number of forces, but the strongest driver is litigation, and the threat of future litigation.
My estimate, plucked from thin air, is that ninety per cent of what is written down is never read by anyone, ever again … ever. The only time anyone shows any interest is if there is a complaint. Then, the interest becomes obsessive, and the management demand that ‘everything’ must be recorded grows.
My other estimate is that medical staff now spend far more time writing, than doing. ‘Doing’ meaning clinical work. Looking after patients – perish the very thought. I have idly tried to work out how much time the physios in our unit spend writing vs. doing. I think it is currently around 80:20.
And what do patients and relatives complain about most? It is almost always that no-one had any time to look after them or pay attention to their needs. I have yet to hear of anyone complaining that medical staff did not spend enough time writing in their notes.
My prediction would be that, if we spent more time doing, and less time writing, there would be far fewer complaints. Because more care could be provided, the patients and relatives would be happier, and so would the staff. Improving morale, and thus patient interaction.
However, this will not happen until we decide to turn the burden of proof round though one hundred and eighty degrees. As I may have mentioned a few times, the current mantra is that ‘if it is not written down, it was not done.’
My counter-mantra would be. ‘We are highly trained professionals, you (Mr Lawyer) need to prove that we did not do our job, properly.’
This does not mean that you can get away without recording anything at all. Clinical notes are still needed. But they need to be clinical notes that are of use to fellow clinicians, not lawyers.
NHS 111 reports should be a few lines max. ‘Mr X has had a cough for three weeks. He reports that is bringing up green sputum, he recorded his temperature at 38.5⁰C. Chest feels tight. No other relevant symptoms. Past medical history of asthma and COPD. Has not yet seen a GP.’’ The end. I need no more than this.
Imagine such a thing. A note that Winston Churchill might have approved of:
‘The discipline of setting out the real points concisely will prove an aid to clearer thinking.’ 1: https://resolution.nhs.uk/2022/07/20/nhs-resolution-continues-to-drive-down-litigation-annual-report-and-accounts-published-for-2021-22/#:~:text=The%20amount%20spent%20on%20claims,billion%20to%20%C2%A3128.6%20billion.

I spent ten years running my own travel clinic, I had some excellent software which enabled me to record my consultations very accurately, and quickly, including prescriptions & written advice given.
In my last (thank heavens) job, as a travel health specialist in a travel clinic, I was required to record in typescript every piece of advice given.
Of course I designed a template & adjusted it accordingly – but what a damn waste of time.
I was always in trouble for not having written enough in my notes – so I gave up & left…
I’ve been helping some friends navigate nhs since 2018. I am 76 but I think I could be a director of my nhs trust (Lincolnshire). As long as they don’t mandate the poison jab. I could make a difference. The friends all say the docs are fine but the admin is terrible. I’ll let you know – Jennifer
So true. This is why, when I had cause to write a pretty fierce letter to the CEO of our local hospital trust, regarding a family member’s treatment, I added a postscript: please don’t treat this as a complaint. And subsequently got a personal call from a member of the relevant department, thanking me for the letter and assuring me that the lesson had been learned.
As for notes: we probably complain more about the waste of time involved than anything else, but of course we just grumble to each other. Another family member’s hospital notes were so voluminous, nobody could ever find anything and I would have to rack my memory to try and tell them what to look for and when it might have been.
It’s as if the NHS is run by people who think Parkinson’s Law was a textbook.
I feel for you. I’m
Dear Dr. Kendrick,
great as usual! I fully agree with your statements – btw I can provide a few “great” examples to the same issue in my field (Mgmt. of semiconductor fabs)
We just are living through a strike of our GP’s here in Germany. They complain exactly about what you describe and our Secretary of Health doesn’t understand, why they are on strike.
At least there will be meeting in Jan. at the federal government level to discuss the matter!
Good luck further!
Hans Harter
Thank you for explaining so well the infuriating waste of time and effort these ‘procedures’ take .Time that could be better spent in today’s NHS .
I was a Heath Visitor for 40 years.
With hand written notes you could record relevant information which hopefully portrayed what you had seen at a home visit or in a clinic setting.
When the computer program was introduced , it became a box ticking series of pathways which to me did not in anyway tell me or anyone else what someone had witnessed or deducted from the ‘client’ contact.
Thank you again Dr Kendrick for your excellent portrayal of life as it is in NHS .
I am so pleased I am retired.
All is written down, except what is accurate, useful and used to be in the notes before they were computerised – like the penicillin allergy that has now disappeared or the pregnancy I didn’t have. Pointless waste of time, I agree.
Thank you for all your work for us. Please don;t let your blood boil!!
A 19 page report sounds more like a tax return. They told us decades ago that the computerization of everything, especially record keeping, was going to de-clutter the system. What a load of crap that was.
Exactly I remember, so what happened to the paperless office promised by the computing (IT) experts as the computers which used to fill most of an average room began to shrink in size due to innovation & advances in technology?
Ah the good old paperless office…
It’s been replaced by kompewters…
Now how much energy is spent on running the servers holding all of these reports that nobody reads…
Answers on a postcard… if you remember them
Is anything actually written down now? When you go to visit someone in hospital, there are no charts, notes, medications or anything clipped at the bottom of the baed anymore. Sometimes there’s a small whiteboard above the bed with something like Nil By Mouth written on it, but otherwise everyone has to log on to a computer to find out when they last ate, had medication, saw a doctor. If the system goes down, everyone is stuffed.
Couldn’t someone design a form along the lines of Churchill’s letter so that the important information is condensed to a couple of sheets of paper? Like my Mum used to use 70 years ago in the NHS …..
Socialized medicine never works. NHS is such.
Nor does corporate medicine. See USA.
True in both cases- the major, leading countries with the most extreme (!) forms of healthcare (HC) at the opposite ends of the spectrum: UK & US have the worst outcomes for patients in dealing with the major killer illnesses. Those with social insurance based schemes like France have far better, the best records for patient care.
Quite right and well said.
<
div>Mind you, even
“The function of medical records is not for them to be written in such a way that they can be used to defend against litigation. It is to pass clinically important information between medical professionals, to enable them to do their job better”.
That is exactly the point. Who decides what should be the function of medical records? Patients, doctors and nurses no doubt agree with Dr Kendrick. But it is not they who have the final say: it is the (boo) managers and administrators. Or “deadwood” as I call them.
Until the NHS is run in the interests of patients, doctors, nurses, and other useful people, things will continue to get worse.
Job justification is the ultimate motive…
Imagine if the number of forms was reduced by 80%…
Won’t need many managers then…
BRAVO!
Well Dr K is right to a point but it’s too easy to blame bureaucracy and management, which generally follow incompetence by over reacting or inappropriately reacting to it. Our local hospital has yet again been deemed “requiring improvement” because not only were records not up to scratch but basic stuff like feeding and watering the patients and making sure IV meds were not way out of date was missed. (And other stuff.) However the job somehow gets done but how many patients suffer and how many staff are failing under the strain of increasing patient numbers is anyone’s guess.
The record problem could be solved if we truly has a NATIONAL health service with standardised and transparent electronic system. Agency nurses come in from out of area who have to be attached to HCAs with the access and the knowledge.
Oh and then there’s the issue of it being better to have the wrong outcome by ticking the right boxes than the other way around.
The point is, that blaming bureaucracy and management is the right thing to do. It IS their fault.
Standardising things isn’t the answer, standardisation stifles improvement. If you set up a set of rules across the country, changing them is almost impossible. The EU has standardised phone charger cables – there will now never be a better cable invented as the cost of getting to market through the regulators is prohibitive.
Nor can you have a transparent electronic system. Have you ever tried using someone else’s spreadsheet? It requires a lot of time working out cell formula to determine how the sheet works. A national transparent system for something this large is an oxymoron. Even the notes will be an issue with regional differences in word meanings – ah, but of course, we’ll have standardised word meanings ….
There are good things and bad things about standardisation. The management of cardiac arrest in hospitals is standardised and rightly so. It is done by a team who do not normally work together but come together for this event. Everyone knows their role and the treatment follows best practice. Better practice should come along with proper trials. not individuals experimenting on patients as they feel like. There are other instances of appropriate standardisation, like very rare conditions a doctor may only see once in a lifetime, or very complicated treatments where it is important to get every aspect correct.
I wouldn’t use the word standardisation. Humans, and diseases, do not come in stanardised packages. I would tend to, agree, that we call it best practice. Remembering, at all times, that there has never been a randomised controlled study on CPR, primarily because it is not possible to do one, so we try things out.
We do also experiment, and if there was no exprimernt, there would be no progress. The first attempts at defibrillaion were a pure experiment. It may, or may not, have worked. The first kidney transplant was an experiment, the first blood transfusion, the first stent, the first use of penicillin etc. etc. You cannot do trials on many, many, things. You try things out. They may, or may not, work.
Yes I agree many medical advances in the past were pioneered by those who thought ‘outside the box’. Of those you mentioned, skin grafts and blood transfusion were first tried out in the 15th and 17th century respectively. The place of the lone experimenter is limited now. Possibly the worst example of physicians ‘doing their own thing’ was Halstead’s radical mastectomy, a massive mutilating operation for breast cancer that did not increase survival compared with conservative surgery. The practice lasted almost 100 years from the 1880’s onwards. I think it is an advance that new treatments should undergo some sort of trial rather than someone ‘sucking and seeing’, especially if you are the one on the sharp end of the needle.
Dr. Kendrick, so under the current paradigm we might as well replace Doctors with AI-robots, couldn’t we?
That would appear to be the end-point we are heading for. There seem to be many who would cheer this on.
Maybe clinicians with a good track record should be given a license to innovate.
AI and surgery… Emmm let’s think about that…
I work in IT and it’s necessary to Alt-Cntrl-Del computers to clear and restart them…
Would the AI robot need to be Alt-Cntrl-Deleted in the middle of an operation…
Only for the brave I would suggest…
But the problem with trials is that they are very cumbersome things to do. Funding, criteria, ethics, paperwork, approvals …..
The problem is fear of being blamed if something goes wrong. But if an experienced professional, or even an experienced non-professional – or even an inexperienced non-professional comes up with an idea that seems sound, why not try it? How do you know that the standard procedure is not more harmful than the considered change?
Toyota used this concept of continuous improvement in the 70s. They abandoned the suggestions box, and (shock horror probe!) gave the workers the authority to make changes as they saw fit, if it would improve the process. This was a major driver in Toyota becoming the leader in reliable, safe, more economical and cheaper cars. I’m sure mistakes were made along the way, but everyone in the world now benefits.
My wife had a problem with an ulcerated cornea. It wasn’t a issue in daytime as the eyelids would blink together, but at night the right eyelid (nerve damaged by a tumour) would drift open and remain so. Her neuro-opthamologist said it would have to be sewed shut (standard operating procedure), but fortunately the surgeon was just about to take a fortnight’s holiday and couldn’t do it that (Friday) afternoon. So we came up with the idea of taping the eyelid down at night. Within the two weeks the ulcer reduced in size by two thirds as the eye was properly lubricated at night, and the operation was avoided. The neuro-opthamologist thought it was brilliant, and now calls me Doctor. Here the SOP was infinitely riskier than a piece of medical tape applied every night, there was no downside to trying it during the fortnight waiting period – yet you would have forbidden it as not being a proper trial and not best practice?
“How do you know that the standard procedure is not more harmful than the considered change?”
You don;t. You would be betting on the odds. In my experience in hospital practice, if I were approached, especially by a surgeon, who said “I have this great new idea”, I would not be the guinea pig.
“My wife had a problem with an ulcerated cornea. ….” Weird! That is just a straight lack of common sense. Are you somewhere that you would have paid for this operation? This could well have been an issue if so.
What was weird? Do you mean that in the UK the eye would have been taped, and that senior Aussie specialists are unaware of the technique? “Yes” is a perfectly acceptable answer – see below. Obviously the operation would cost money, how much would have been covered by Medicare and how much we would have had to pay we never found out, but wouldn’t have been an issue for us. It might even have been covered by her hospital health insurance.
“I have this great new idea”. You have a meningioma on the base of the skull. It has encased the optic nerve, a basilar artery and is pressing on the brain stem. It has pretty much destroyed the trigeminal, 6th and 7th nerves. The SOP is to remove the ear and the roof of the mouth to access the tumour from two directions in an operation lasting 12 hours. Recovery time is three months minimum, although you won’t recover the use of your ear (balance, hearing). With three young children it’s a daunting prospect, especially as the only outcome one of the butchers can give from his nine operations on similarly positioned tumours is that of a woman in her mid thirties who lives a ‘reasonably independent life’, whatever that means (can control her own wheelchair?)! The stats show that all meningiomas regrow, and 46% reach their pre-op size within 20 years. Radiation causes swelling of tumour in a third of cases, and is no more effective in 2010 with IMRT, gamma knives, proton beams etc that waving a lump of radium in the vague direction of the tumour was in 1960. Along comes Charlie Teo, who had heard of this great new idea of keyhole surgery in the US and gone over there to learn how to do it. The butchers hated him to the extent they’ve now forced him to stop practising in Australia. However we went with the great new idea with zero recovery time (op finished at 11pm, discharged 8am, flew home next day) and after 13 years no regrowth – it actually looks as if it has shrunk slightly.
OK, so it wasn’t a brand new great idea, but it was new to Oz, and the pushback we were getting from the butchers and radio-oncologists was enormous, just as though it had never been done before.
Notes!
No one looks at them. I couldn’t agree more. (I think teachers are supposed to write something, about every student, in every lesson.) It’s beyond utterly nuts.
Each time I visit the surgery I’m seen by a new Doctor. I understand they’re supposed to understand everything about me, from notes.
Yet what they then do is to go over once again everything that has happened to me, and we re- join “the diagnostic pathway”. More like a ‘diagnostic roundabout’ actually.
After several months of this I am insisting I join “a treatment pathway” in order to heal and become healthy again.
Andy Lowings
Has this become worse? I recall being very frustrated by the pointless, and wasteful, demands of managers to record far too much, analyze, compute, etc. etc., as far back as the 1990’s. It was a great day when I retired in 2010 and I have never looked back at what had become a service for managers rather than a service for ill people. I now live in a country where doctors see two or three times as many patients as doctors do in the UK. Their notes are very short and factual and are completed with the patient present, with a copy given to the patient.
I do wonder whether the complaining by the public is worse where the health services are given freely. I have to pay a fee to be part of the health insurance and this payment does confer some sort of respect for what is received.
After a blood test a week or so back I was phone by a GP from our local Medical Centre. Conversation went like this:
GP: The test showed you are pre-diabetic and have high cholesterol. I’d like to put you on a statin.
Me: I’m not going back to statins. I gave them up many years ago.
GP: Oh, why?
Me: Well, they made me feel ill, and anyway their effectiveness has been grossly exaggerated. Quoting Relative Risk Reduction at patients instead of Absolute Risk Reduction gives a false picture.
GP: Well, you must remember that the trials are funded by the manufacturers so they’re bound to be exaggerated.
Me: (thinks “WTF!”)Pardon??
GP: Well, you might like to consider a low-carb diet.
Me: I’ll certainly consider that.
When a previous GP advised me to read your “The Great Cholesterol Con” and then told me she “wasn’t allowed” to advise me not to take them it gave a glimpse of what must be malpractice in the NHS. I assume they have to suggest statins as a first step whatever their own opinions might be.
At least you got to see your GP! Our 23 y/o son got the ‘flu a few weeks ago, very badly, confined to bed for four days. Never been so sick. So he needed a medical certificate for work. Rings local clinic. “We’re not taking new patients” says the receptionist (I believe she has a diploma, of degree, some piece of paper anyway giving her the qualification of Practice Manager. But she’s really the receptionist).
“I’m not a new patient” says son.
“You haven’t been here in the last twelve months, so you’re a new patient. The last time you came was three and a half years ago.”
“But I haven’t been sick. I’ve been seeing Penny (the doctor) since I was born. Or even before that.”
“Sorry, those are the rules.”
Being so sick he couldn’t argue, but fortunately his seven month pregnant sister (who is actually not sick) had a check-up with Penny the next day, and Dr. P gave her a sick note for her brother. So now we’re all committed to appointments every ten months just to say “Hi” to the doctor so we can maintain our “current patient” status.
The trend is to eradicate any special quality to what doctors and nurses do, and make them indisinguishable from assembly-line workers or farm labourers.
I saw the same thing when I worked in the computer industry. Managers who knew literally nothing about hardware or software dictated to people with PhDs in electronics and software – simply because that made the managers feel good about themselves.
Naturally the company went out of business in a few years.
There is also the consideration that everyone must be sick all the time, to provide job security and maintain Big Pharma’s profits.
Is this in the UK or some other country. I have never heard of this happening in UK, but if it is a new phenomenon. it would seem you have to ‘log in’ to GP every year with a fictitious illness to remain on the books
Australia. And it seems very common here. Unfortunately, our GP is too much of a people person, often spending much longer than the standard 15 minutes per patient so she’s always running late. Fortunately we know her very well and if my daughter hadn’t been going in I would have called her mobile if necessary (we’ve never had to do so for professional purposes yet).
The concept of a “healthy person” seems to have become alien and very much unwanted.
If you are healthy, you do not depend on the authorities.
If only doctors pushed back, perhaps unionized… But white collar people are terrified of that word.
Instead, they inched you all to end up with a paltry 7 minutes per patient.
I kind of blame the culture around these high level professions who stupidly compete with each other….
“The evolutionary psychologist William von Hippel found that humans use large parts of thinking power to navigate social world rather than perform independent analysis and decision making. For most people it is the mechanism that, in case of doubt, will prevent one from thinking what is right if, in return, it endangers one’s social status. This phenomenon occurs more strongly the higher a person’s social status. Another factor is that the more educated and more theoretically intelligent a person is, the more their brain is adept at selling them the biggest nonsense as a reasonable idea, as long as it elevates their social status. The upper educated class tends to be more inclined than ordinary people to chase some intellectual boondoggle. ”
-Sasha Latypova
And I think that was exemplified during Covid with the number of ‘ordinary’ people who refused the jabs. Housewives, electricians, roof gutter cleaners, shop assistants etc. who wondered why they seemed so smart compared to most of the population, as it just seemed to them to be too risky, in spite of the bombardment of misinformation aimed at them by the so called professional classes.
Aaaarghh! What is the way forward? How can anyone extricate the NHS from this turgid bureaucratic foul up?
Abolish it, admit that it was a fundamentally wrong idea, and go back square one: doctors and patients.
That can’t happen, of course, because it would mean admitting that all the politicians and clever social reformers were wrong.
In its broad outlines, the NHS was a marvellous idea. But like so many wonderful ideas in the realm of politics, it fails because the devil is in the details. The NHS is a parasitical manipulator’s dream, which is why it has become riddled with them.
No scheme that fails to take into account the prevalence and capacity for fatal harm of parasitical manipulators can succeed. But theither can we hope for politicians ever to accept that, if only because they themselves are parasticial manipulators who long ago reached the top of the muck heap and now earn a comfortable living, supplemented by generous perks and social deference, for doing essentially nothing – if we are lucky.
“Abolish it, admit that it was a fundamentally wrong idea, and go back square one: doctors and patients”
No it was not a fundamentally wrong idea. The fundamental wrong before is that the poor were denied medical treatment as they could not afford it. The main cause of individuals going bankrupt in the USA is being beggared by health costs. Do you thing this is a good system?
John, I agree that everyone ought to be given appropriate medical treatment when they need it. But the NHS was a fundamentally misconceived way of solving that problem. It suffers from giantism and cancerous growth. Dr Jerry Pournelle’s Law of Bureaucracy fits the NHS perfectly, although he was American and probably not thinking of the NHS specifically.
“In any bureaucracy, the people devoted to the benefit of the bureaucracy itself always get in control and those dedicated to the goals the bureaucracy is supposed to accomplish have less and less influence, and sometimes are eliminated entirely”.
I think it would take a brave (and somewhat blind) person to deny that the NHS has undergone exactly that process. I am well disposed to socialism (properly so called) but in the modern era so far it has usually been attempted on a vast scale by governments, and so has failed. The problem does not lie in socialism itself, but in the fact that almost all government projects fail, and the bigger and more ambitious they are the more disastrously they fail.
At a more fundamental level, many/most people fear chaos. The idea that an individual in an organisation may do things that are not tightly controlled is deeply uncomfortable to the bureaucratic mind. Standardisation…. as someone commented earlier, is required. There must be processes, and processes must be followed. All errors, therefore, represent a failure to follow process correctly. Or, that the processes themselves need to be tightened up, continuously.
This, inexorably, leads to more and more rules and regulations that ‘must’ be followed. It inevitably removes individual autonomy, and turns the workforce into a tool of the bureaucrats/managers. The Henry Ford dream of ‘production line’ efficiency. This is your task, this is exactly how it must be done, there can be no deviation.
This would work, somewhat better, if humans were robots. But humans are not robots. and if you try to turn humans into robots, and remove all autonomy, then they stop doing all the things you need them to do, that humans are very good at. Identify problems on the ground, and try to sort them out. Work with enthusiasm. Find innovative solutions. They lose motivation, they stop caring about the job that they do, and drift. They become deliberate obstacles to getting work done.
This is what dragged down the Soviet Union, and will always drag down big organisations – if you don’t work very hard to stop it happening. It is not necessarily a ‘socialist’ thing. Although my observation would be that left-leaning people seem far keener on the idea that the ‘state/organisation’ must control everything, for the good of everyone. Individual freedoms must be curbed, to control all possible chaos/errors.
With the NHS we see a massive ‘state’ organisation inexorably becoming a more and more massive bureaucracy with ever more rules and regulations to ‘control’ everything. Those working for it become, in parallel, less and less enthusiastic about their work. They come in, they do what they are told, they leave.
If the NHS was a private company it would have gone bust, long ago. But it has no need to worry about funding. It keeps getting that, no matter how sclerotic it becomes. Therefore it cannot ever ‘fail’. Without any requireemnt for financial discipline it will grind on unchanged, forever, I suspect.
In response to what you and MK in his reply below, I have not experience of UK GP practice. My experience is entirely in hospitals, and I suspect GPs are much more encumbered by regulations etc than we were.
I sat on the hospital Local Negotiating Committee, the doctors union body. Policies would rain down monthly from above, most to deal with a small or perceived problem using massive sledgehammer to crack a small nut. These policies essentially existed in a parallel universe, because, unlike the impression from MK’s reply below, at the ground level, all the staff would work flexibly, use initiative and intuition to make the system work and get the work done. Obviously, this was within limitations of what was possible, but no-one worked as robots. We had to pretend to follow the policies, and they pretended to believe us. Of course, if something went wrong, inevitably you were first in the firing line.
As Dr. K has so clearly exposed, you also have to add the problems of providing a “free” service with limit resources. For any government this will naturally lead to over regulation and stiff controls. The greater the limit resources the bigger the stiffer regulations. To that you have to add the special interest that always are behind the politicians and bureaucrats buying influence so that their interest are serve first, one big example the COVID farce.
I have lived under both system with “free” services even do on a place with very limited resources and the USA system and after COVID I without doubt prefer the latter. The USA system is not perfect as no system is but if not as bad to how is often portrait, with no help for the poor, for me is better compared with the alternative.
Serendipitous that you should mention Ford, Dr Kendrick. I have just been reading a rather good sociology book from 1974, and I came across this quotation:
‘”Every man knows”, a study of the Ford shops once reported, that “the door to the street stands open for any man who objects in any way, shape or manner to instant and unquestioning obedience to any directions whatever… wilful insubordination is, of course, absolutely intolerable, and Ford workers must, first of all, be docile”. That was written in 1915 by two efficiency experts, and even those kind of people don’t say such things in public anymore’.
I don’t know how you and your other readers feel, but when I read those words my immediate, automatic reaction was a wave of furious resentment. I am a free man, not a slave. I am perfectly willing to work for anyone who pays me reasonably for useful work. But not for anyone who takes that attitude. I suspect that the demand for “docility” had – and has – far more to do with the personal emotional needs of managers than with any practical necessity.
“…if you try to turn humans into robots, and remove all autonomy, then they stop doing all the things you need them to do…”
As the joke went in the USSR, “you pretend to pay us and we pretend to work”. Russia has moved on very far since then; but Britain seems to have gone backwards.
Since doctors can and do go on strike, why can’t they organise ‘industrial action’ that involves only writing notes containing relevant information? That way the patients wouldn’t suffer – only the managers!
Great idea! That way the GP waiting lists
(where the obstructors have least influence) would disappear within a fortnight.
I live in the US and don’t know of anyone being beggared by health costs. Rather, I see problems with insurance denying legitimate claims. This all started with ACA.
Al this pointless data gathering could be because THEY think that feeding the results into their AI machine will allow it to diagnose conditions more accurately. I think it would not help anyway as the data may be rubbish. Who is to know whether the answers to the questions are accurate or even truthful. If I had to answer 19 pages worth of questions I would have topped myself way before the end. Vitamin D, vitamin C, zinc, sodium, potassium, and a few other inputs, supplement or preferably proper food, and for most people just put up with what you’ve got. Likely it will pass in a couple of weeks. I hope castor oil is helpful as that’s my next gambit
Sorry Dr M, but sometimes I disagree with you.
I have been following and replying to your blog for a couple of years and most times I agree with you but sorry not this time (well not fully).
Whilst I agree brevity is everything, A4 max to get data/an idea across, sometimes however…
Yesterday I spent 5 and a half hours in A&E with my wife (73 years old), we got an appointment with our local GP, after I answered as you say an interminable list of questions on 111 which could easily been simplified I.e. had she had a stroke, face dropping, etc. (NO) had she had a heart attack, arms in the air, etc. (NO) but these are important referrals to a more serious 999 call, yes it is all about diagnosis, what is serious…
The local GP after a lot of prodding and measure said basically she though there was a problem and to be safe I should take her to A&E, and she would forward her notes (from watching what she typed about an A4 sheet).
A&E (Taunton) was a revaluation the organisation was A1 !
We got to see a a triage nurse in 15mins, with lots of notes taking,
An ENT doctor within 30 mins, again with lots of notes,
Just looking around A&E at the patents a young lad with with broken arm was treated brilliantly,
A women who came in with a small gash on her nose had to wait (lots of bloody but minor really),
A women who came in in obviously with server abdominal pains was admitted virtually mediately.
To my short observations the system has got it right!
My experience would suggest, it might not be efficient but at least it is working for patents that need it, perhaps the emphasis should be improving what what exists rather than complaining about the system as it is (which unfortunate we all do about most systems).
The doctors spent a lot of time asking about my wife’s medication, as to what to proscribe for her illness, I did a lot of reading online afterwards, I think they got it right (I have a strong science background so could understand the drugs they suggested for her and why).
I think the problem is not just lawyers but people in general are becoming educated, which is good because the medical profession has also rise to the challenge of being better at their job.
My experience of yesterday suggest documentation is necessary, it does save time, and stops doctors asking the same questions over again.
As to your concerns….
Perhaps we should just do what Shakespeare suggests and kill all the lawyers.
A visit to local A&E last month late on a Monday night found the waiting area over-crowded. A doctor came out and told everyone “We have 180 patients waiting and a queue of ambulances outside. Please, if your condition isn’t life-threatening and you can contact your GP in the morning, please leave.” No-one left, but all turned to the person next to them and I could hear them justifying why they where there and “isn’t it dreadful how you can’t get treatment”, etc. A woman sitting by me said she had a cough that was making her throat sore and “had to have antibiotics immediately.” (I was supporting someone who had seriously self-harmed).
Your frustration is palpable and embarrassingly I recognise my student nurse self of 55 years ago writing lengthy patient notes at the end of each shift.
Then again, my note taking after conducting a staff performance appraisal 30 years ago saved me when among other factors, the hospital was taken to court by the appraised nurse on another matter. I was among those summoned and my notes demonstrated that this nurse was a vexatious litigant.
Regardless, you are spot on. Documentation and quality control has gone mad. Whole careers are now built on them and suck away hours that used to be spent on actual patient care.
I am with you 100%. It makes me cringe to think of all the paper work I had to do, not to mention the meeting…… Only a third if our time was with.a mental health patient. How sad is that. I only worked in that area a few years and hung up my boots for good. Hate to think what it’s like 11 years on…..
Great item. Keeping it brief 😀..How is your health??
The mantra actually makes it so that important things are not written down. I am yet to see anyone who is willing to spend anytime to fill in and follow up on so called “minor incidents”. Verbal communication has completely disappeared, which in turn makes it impossible to provide/receive adequate care.
It is,as you say, a sickening trend to do all this useless writing in the name of protecting against litigation. I work as a phlebotomist and could say for sure that 90% of the requested daily tests are not necessary and in anyway helpful to the recovery, but only done “for the record”. The whole thing has become even worst with the computerisation…
I have retired from a GP job which included looking after in patients in a community hospital. We had to write our notes in the same section as every other discipline. It was supposed to show how things happened in chronological order. The trouble was that as a group doctors still wrote much less each day than all the other disciplines (except the newly qualified ones, who wrote 2 pages) that it was often difficult to get a meaningful idea, from the medical point of view, of the patient’s journey. Often there was nothing to say, but you couldn’t write that, so entries by doctors would be variations on ‘comfortable’, ‘stable’, ‘no real change’, ‘obs stable’ – basically any proof that you had seen the patient that day.
Even when something clinical happened, it was usually brief, like ‘deteriorating’ ‘died ‘ (passed away for the euphemism addicts), with a time, and cause of death to speed up writing the certificate.
From today’s “Daily Sceptic” (recommended):
“I Experienced the NHS’s ‘Innovative’ Use of Technology to ‘Improve Efficiency’ and Ended up in an Endless Loop While my Symptoms Went Untreated”
https://dailysceptic.org/2023/12/28/i-experienced-the-nhss-innovative-use-of-technology-to-improve-efficiency-and-ended-up-in-an-endless-loop-while-my-symptoms-went-untreated/
“Knowing the challenges of securing a GP appointment by telephone, I physically visited the surgery on December 12th and was pleasantly surprised to schedule an appointment for December 14th.
“Understanding the severity of my condition, my GP booked an MRI scan, assuring me of a text within two weeks for confirmation.
“However, instead of an appointment by text, on December 26th (a full two weeks after visiting my GP) I received a perplexing message about a “physiotherapy referral” and a link to complete a digital assessment via Phio, an NHS automated chatbot.
“This process took an agonising 40 minutes with a myriad of questions and instructional videos of how to move my arm to test symptoms and seemed utterly pointless since an MRI was already deemed necessary by my GP”.
A good, dedicated and diligent GP friend of 64, who was a teacher of GPs, got hounded out by one particular non medical bully of a ‘supervisor’ because he couldn’t write the bilge they wanted him to. When he asked her how she wanted him to answer the questions she told him it was up to him to work it out. She said he had the wrong attitude. She said he had a mental health issue – now he’s not working for the NHS anymore he no longer has a mental health issue.
Also, in the Waterlow assessment there is not one question about the emotional state of the poor benighted patient. Dear God!
Computerisation has a lot to answer for. It is not peculiar to the NHS. When drawing up user requirements for a mechanised system, all user requirements ( usually) are catalogued. The programmer has limited ability to assess the importance of the expensive list of requirements. Especially if he or she has limited knowledge of the requirements or ways of working in the organisation, as usually is the case with external consultants. Unless you curtail this process no new system will ever be implemented. Unfortunately, in the interests of efficiency this difficult process is often shortened to prioritise the objectives of the project leader or their superiors.
Some important items are missed while other spurious requirements are included. Just because something can be measured does not mean it should be included.There is always a tendency to require too much of the system. The more levels there are in the organisation the mote likely the system will be strangled with data. In theory, data management will make relevant data appropriate to each user level as required . In practice everyone, or at least senior management, has access. one way or another, to everything, particularly where potential litigation is involved.
The further away the project leader is to the coal face the less likely the resultant system will satisfy the front line users.This is a fundamental law of computer systems.
When GP’s are looking at computer screens rather than patients then this is evidence of a poorly designed system. When sales staff are writing reports on line rather than talking to customers then this is evidence of a poorly designed system. When logistics staff are spending their time feeding the system rather than prioritising delivery then this is evidence of a poorly designed system.
It is tempting to think that better design will sort out the problems but no computer will ever substitute for a smart human being. Yes data will help but only if it is appropriate for the users needs.
I completely agree, jsmith. As someone who has been teaching and writing about software and computer systems for 40 years, your comment reminds me of the well-known apocryphal saying (well-known to computer people, anyway):
“At the source of every error which is blamed on the computer you will find at least two human errors, including the error of blaming it on the computer”.
Primum non nocere – ‘first do no harm’.
Then along came covid and that went out of the window.
Basically, the GPs and staff at my local surgery lied to me. And presumably many other local folk too. I asked our Practice Nurse, a wonderful lass who I like and admire, if these jabs were really doing any good or is the diametric opposite. She just looked me in the eye and didn’t answer. She couldn’t, could she? She has a family to feed and a mortgage to pay.
Approx figures here: Within the NHS there are around 150,000 doctors, 60,000 consultants, 375,000 nurses in addition to 1,000,000 ‘others’. With the exception of a tiny fraction of this 1.5 million, they all lied, blackmailed and conned us. Still are. As we know, one of the exceptions is the writer of this blog. Thank you and long may you continue.
(The budget for all this lot is about £170 billion paid for by me. And you, of course.)
How much influence, as a collective, could the vast number of medics have had if they’d just had courage? The opportunity is still there.
Regarding the jabs, some sense seems to have seeped through because it is the great unwashed who have decided to forego further ‘interventions’. If it was up to the establishment we’d still be being shot full of holes.
The upshot is, how are we, customers turned victims, supposed to trust the medical profession ever again? That’s a horrid, sickening thing to say, enough to make you poorly. But, whatever outside pressures influenced medical practitioner’s decisions and choices, there was simply no excuse to put us in the firing line.
YES! But the reality is that it’s not about the jab/s per se, it’s about CONTROL, of us through FEAR (nudge, nudge).
Not verbatim conversation with someone from my local council, sometime in 2021:
Council: “Hullo, I’m phoning you from ******* Council about your Covid 19 vaccine that we’re offering you”
Me: “No thanks”
Council volunteer: “You don’t want it?”
Me: “No, I caught it in December 2020″
Council (Shock, Horror): And you’re still alive?” (I was 76).
Me: “Obviously”
End of conversation.
Unfortunately yes. Whilst having never taken anything a doctor says as an absolute truth, their reactions to covid where they deliberately withheld safe medications and cynically injected toxins after the trial results showing a 23% increase in deaths and 70% increase in hospitalisations in the “vaccine” cohort have destroyed any trust.
Yes, they have mouths to feed. But no conscience (our GP, who owns her clinic, refused to give the jabs).
“She just looked me in the eye and didn’t answer. She couldn’t, could she? She has a family to feed and a mortgage to pay”.
Right there, Jeremy has summed up the worst thing about the NHS. Those who can practice medicine effectively try to do so, but they are continually obstructed and sometimes – as in this case – actually forbidden to do what they know to be right.
The only way to get the NHS (or some successor) back on the rails is to make sure that never again can any overpaid ignoramus in a suit forbid a trained doctor or nurse to treat and speak to their patients as they think best.
Wow having just read all the comments you have really open a can of worms with this blog, there are some strong views expressed.
From the start I will state there may seem to be a conflict of interests: I worked in the computer industry for 40 years before retiring, as a programmer, software/system designer and finally in management, so I disagree with many of the comments expressed about computer systems and big data collection, but ignoring all that, lets begin:
If you want to do “Evidence Based Medicine” you need Evidence!
Evidence is Data!
One of the best ways to collect consistent data is using forms, it makes processing easier.
Using the old school approach of abbreviated personal notes for data collection is a nightmare.
OK it is perhaps reasonable if you have a few patents you know, but when it comes to dealing with medicine for large populations who you don’t know, you may be missing just so many opportunities. Data in a structured form is absolutely vital when dealing with any large complex system like people and diseases for example!
Why do you think for big players want to buy the NHS data for billions! Data is valuable, extremely valuable!
We are at the cusp of incredible changes in understanding in medicine (and many other areas), in cause and effect, driven by big data and new analysis techniques.
Can I suggest your readers watch a YouTube lecture by Norman Fenton on “Bayesian networks for healthcare data” (not an easy watch but very interesting).
And also read the book by Judea Pearl “The Book of Why” on Causal Networks.
These are new ideas, circa 7 years.
Big Data and these techniques are going to change many things in a big and very positive way, including medicine.
Watch this space as they say…
Roy, I to have a similar background to yours, however; I am not so optimistic about the big data driven future ‘they’ have planned for us.
In theory, AI and big data will open the door to advances, some of which we can already see: eg.breast scans. The problem is always who has/owns the data and to what use will ‘they’ put it ?
The current big data gatherers such as Google, Amazon, meta, etc. have shown over the last several years how they collect, manipulate and misuse their data. Has this really made our lives better ?
Medical data will be no different, IMO. It will be misused by the collectors (Gates, big pharma, et al) and used to further ‘their’ agendas (WEF, UN/WHO). and none of this will be free to us. We will have to pay for medical advances that are based on our data !
As 2024 begins I’m not optimistic that things will get better. I see a future that is markedly worse than how we lived in 1974. We have not progressed, just the opposite.
Could you expand on your statement about data facilitating advances with respect to breast scans. How has the data advanced treatment and in what way?
I initially saw this reported in a programme several years ago. AI had been trained to analyse breast scans and detect potential tumours. The success rate was reported to be as good as or better than currently achieved by specialists radiologists. Obviously, the training data is crucial and specialists have the final say.
There’s plenty of reports available if you Google the subject.
Unfortunately google is not known for unbiased suggestions, for example if you look up mRNA vaxes, there is much that says how safe and effective they are, and conversely how dangerous vitamin D is. Do you have a specific report in mind?
AhNotepad.
Sorry, you’ll have to do a little research on your own. The fact remains there are some potentially good uses for AI as I’ve suggested, but the issue is data ownership and misuse. If you believe I’m wrong feel free to explain. Otherwise, with respect, I have better things to do.
Roy,
I have a hunch that as part of your job, you probably gave motivational talks to health service managers. I expect your talks were greatly appreciated, so it must come as a shock to read the discussion here.
Some people here are doctors and nurses, while others, such as myself, came here because of an NHS fad for prescribing statins. If you want to discover why statins aren’t such a great idea (except for Big Pharma), I suggest you read Dr. Kendrick’s book “Doctoring Data”. It will show you in great detail how things go wrong, so I’ll just whet your appetite. The effectiveness of statins in preventing cardiovascular disease can be presented using absolute or relative statistics. In absolute terms they are at best approximately 1% effective, but in relative terms they are over 30% effective. Needless to say, the low figure is relevant to individuals, but it is the higher figure that is usually quoted because it is relevant to Big Pharma. That is where following the data can lead.
Roy, you say…
“Why do you think for big players want to buy the NHS data for billions! Data is valuable, extremely valuable!
We are at the cusp of incredible changes in understanding in medicine (and many other areas), in cause and effect, driven by big data and new analysis techniques.”
Unless I’ve got the wrong end of the stick Dr K is saying that time spent filling in ‘unnecessary’ details is time not spent treating patients. He’s coming from a clinical viewpoint, which is what we want when we go and see our GP. He doesn’t need to record the fact that I am the owner of two dogs and travel by train once a month – stuff completely irrelevant to my treatment (but possibly valuable to a train operator).
In addition, if doctors are data-gathering as a commercial activity, that is not exactly what I believe to the the raison d’etre of the NHS (which is funded by me and you)!
I also think you’re missing a crucial link in the chain. Namely, we, the public, will only ever hear about what those in power (those who hold the purse strings) want us to hear.
PLUS much of the data published in recent years has been utterly skewed by lack of transparency and scientific debate. Spurious results based on the sole premise of selling more ‘product’ published by institutions who have enjoyed a little financial lubrication. Basing new treatments and medications on false data is worse than no change at all.
(There’s a very good interview with Professor Angus Dalgleish with John Campbell on You Tube during which he speaks of cancer treatments he’s developed that are being held back. Results that won’t be data-recorded because they are ‘not allowed’ to be.)
The data that are gathered are very difficult to interpret, and are often completely wrong. I spent some time looking at angina, and patients with angina. I found many patients had a record of angina, and this was one of their significant problems. In once case the consultant had said ‘this patient does not have angina.’ But the word was seen in thier notes, so they had angina, recorded, never to be removed. You often find patients are recorded as having an allergy to penicillin, when they don’t. Around 75% of those with a recorded allergy do not actually have an allergy. If you want to understand medicine via big data, then you really need to know if these data mean anything.
I would also be interested to know what these incredible changes might be? Diseases are due to genetics, the environment, and lifestyle. You can analysie big data any way you want, and that ain’t going to change.
Another problem, close to my heart, is that big data will confirm that cholesterol causes CVD. But it doesn’t. In my view all that big data is going to do is ensure is that the current disease paradigms become locked in – forever. Amyoid proteins cause Alzheimer’s…. no they don’t.
QOF – the use of EBM to drive improvements in preventive medicine – has achieved, exactly, nothing. Big data, analysed by super clever computer people who have never seen a patient in thier lives – and never will – will miss almost everything that is important. and will never believe this is so. As Einstein once said. ‘Most things that can be measured don’t matter, and most things that matter can’t be measured.’
Hi Malcolm In The Great Cholesterol Con’ you noted that increased saturated fat intake in Japan resulted in an increase in cholesterol levels and a reduction in strokes. Does this suggest a link between saturated fat intake and cholesterol counts? Your book is a favourite of mine and it is just this point that bothers me. Kind regards David
Sent from Yahoo Mail for iPhone
There is a major confonding factors here. Actaully there are many, but will stick to one. If you eat a lot of vegetables, thus a lot of vegetable sterols/stanols, these interfere with cholesterol absorption. Plant stanols are almost identical to cholesterol. Thus, the liver has to synthesize more cholestero to meet the bodies needs, and needs to reabsorb more LDLs from the bloodstream to create the VLDLs to transport fat(s) and cholesterol to the rest of the body.
Thus increased plant consumption does lower ‘cholesterol.’ However, increased saturated fat consumption does not increase it. It has no impact. Thererfore, as the Japanes reduced vegetable consumption, and increased saturated fat consumption the LDL (and thus totatl cholesterol levels) did rise. This was due to the reduction in vegetable consumption, not the increased saturated fat consumtpion. A subtle point, to be sure. But critical to understanding. Thus, the MCE trial in the late sixties, showed a reduction in cholesterol levels when saturated fat was replaced by vegetable oils. It also showed that reduced cholesterol levels were associated with increased risk of CV, and overall, mortality.
The problem with almost all nutritional studies is that you are – almsot always – changing two variables at the same time.
I see the great John Pilger died yesterday.
Thank you so much for explaining this. The holiday is my time to catch up on reading. I have bought a copy for my son this Christmas and recommended it to a friend who lives in Macclesfield.
Hi Dr K,
Well Happy New Year to you and your good bloggers – and thanks for this helpful clarification in answer to DavidTucker59, (great question)
This seeming conflict has stumped me for a long time too. I never would have extrapolated that there were 2 dietory factors at work and the hidden one – eating less vegetables – was what ACTUALLY caused cholesterol levels to rise, not the eating of more saturated fat.
Makes sense, studies of ancient cultures inform us that their diets were 80% vegetable and I’m not sure if it’s connected in any way but meat is the only thing chimpanzees share.
Not if they were Inuits, and probably some Siberian natives and maybe Masi. If they had veggies at all they were probably less that 80%, and possibly by quite a bit.
I am going to disagree here. Ancient cultures ate many different diets, including diets that were almost purely animal based. More recetly, we have the Inuit, who never ate a vegetable in thier life. Or the Masai, whose diet (for men) was meat, blood and milk – entirely. Until the start of agrarian based societies, most humans ate a lot of meat. Cave paintings from fifty thousand years ago do not depict humans hunting brussel sprouts.
Hmmm, I wonder if the veggie supporting studies were references provided by, er, google.
Ahhh. I’m glad to have the opportunity to set the record straight.
Cave paintings depicted early humans hunting animals – correct. But the misconception is that they were subsequently eaten – they weren’t.
The hapless beasts were tied to stakes outside caves to lure in the sprouts. The sprouts would be snared in nets, bundled into family-sized portions and distributed throughout the ancient world via corner shops.
😂😂😂
There is an exceptionally good book on this subject “Nutrition and Physical Degeneration” by Weston Price which describes expeditions in the 1930’s to many place around the world looking at the problems of the introduction of sugar and bread/wheat into the diets. The native diets were incredibly varied! Some Like Dr K saves had virtually no veg. Some had little meat and veg but lots of sea food. Worth a read at £20 or so.
Qualified writers such as Dr Shawn Baker explain very clearly and simply that, while many carbohydrate foods are palatable and somewhat nourishing, none of them are essential to human life. For perfect health, nothing is necessary except good quality meat (fresh, fatty) and pure water. The meat may optionally be cooked, but that is not essential if it is of good quality and low in pathogens.
Protein is needed to keep the body’s structures (bones, muscles, sinews, organs) intact and healthy. An often-cited amount is 100 grams of complete protein, obtainable from about 1 lb of beef (or equivalent).
Saturated fat is the ideal fuel for all cells (except, perhaps, the brain – which is often said to require glucose but which also does well on ketones derived from… fat). It’s little known that animals such as ungulates, which eat only grass and other such vegetable matter, have bacteria in their stomachs that convert all the vegetable matter into saturated fat. Cows, horses, sheep, goats, etc. live on almost 100% saturated fat!
Carbs may contain some nutrients – many do – but they are basically empty calories, which are not needed if enough saturated fat is eaten.
Of course none of this has anything to do with preferences in food. If a person loves doughnuts or rice, they may choose to eat those foods – and probably suffer little or no harm, in moderation. But they don’t need to.
This was discussed in a previous post but I included here so it seen more. Even Dr. Mercola has change his opinion on very low carb diets and his opinion on Ray Peat ideas. (Just for information to provide another point of view)
https://articles.mercola.com/sites/articles/archive/2023/12/31/bioenergetic-theory-of-health.aspx
Story at-a-glance
While insulin resistance is routinely identified as a root cause of most chronic diseases, it too is only a symptom of a deeper problem. At the root will be impaired cellular energy production in the mitochondria
Insulin resistance occurs when the cells are unable to properly oxidize or burn glucose
When your body shifts into fat burning this results in lowering your metabolic rate, which is antithetical to optimal health. For optimal health, you need a high metabolic rate, and this is facilitated when your metabolism speeds up when you’re burning glucose in your mitochondria
A general baseline for most average-sized people is between 150 grams and 250 grams of healthy carbs per day. If you’re very active, it could be as high as 500 or 600 grams a day. Keep in mind that as you increase carbs, you also need to cut down fat. Fat intakes above 30 to 40% or so of daily calories will tend to inhibit glucose metabolism
Healthy carb choices include fresh whole fruit, fruit juice, root vegetables such as potatoes, sweet potatoes, parsnips and carrots, white rice, raw honey and maple syrup
—-
In this video, I interview independent health researcher Jay Feldman, who has a podcast called “The Energy Balance Podcast.” I recently came to understand the importance of the late Ray Peat’s work, which I had previously dismissed for over three decades, largely due to confirmational bias.
Peat was a biologist and physiologist, and a cofounder of the prometabolic diet based on the bioenergetic theory of health.1 After re-exploring his work, I’ve come to realize just how ahead of his time he was. Feldman is among the few health researchers out there who has also embraced Peat’s work and understands it at a level that allows him to explain it in layman’s terms.
If you can’t access the Dr. Mercola link here is an alternative but you will miss Mercola point of view.
https://www.jayfeldmanwellness.com/
I’ve done out of hours work and heard 111 call handlers in the background and I agree with MK it’s mainly an endless list of negatives , I’d joke ‘not been struck by lightning…’ and yes when you see the patient subsequently you struggle to extract meaningful info from the reams of drivel , then pretty much start again with a focused history etc. I’m not there now but did sessions in an out of hours where random consultations are reviewed and commented on , and while I agree it’s important to document the clinical findings etc there really was an emphasis on record keeping that could disprove subsequent complaints of missed diagnosis etc but this leads to endless defensive minded documentation of no this no that etc. Heaven forbid being able to describe a child as ‘completely well’ , after 20 years of being a GP and over a decade in hospital medicine prior to that it’d be nice to be able to apply some common sense to the documentation. I’m now working in Australia and I do observe a huge variation in quality of documentation from the practically non existent to ludicrously detailed. Needs a happy medium
Ummmmm, excuse me, but it appears that there may be no “vaccine” or anything to cure the NHS, so may I take a moment to ask, however impertinently, the good doctor his views on using paxlovid to do something about “covid?” It seems to be all the rage here in the US now and surely that cannot be a good thing. (Either the rage or the medicine.)
Thanks, and blessings to all! : )
• Apolipoprotein (a)
• Heart Disease
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6067813/
Is this off topic or on topic? Lp(a) has been a fascinating topic here and a little known one in general.
What’s wrong with the NHS ?
Well here’s another couple of examples:
1. Over the last decade, NHS England spent £13bn on just ten super-expensive drugs. (That’s £130 Million per drug per annum, or £356,164 per day);
https://www.declassifieduk.org/if-we-want-to-save-the-nhs-we-need-to-take-on-big-pharma/
2. The failing Princess Alexandra Hospital NHS trust, which ended last year with a deficit of £13million, has been accused of “slapping taxpayers in the face” after it blew £58,000 sending 14 members of staff on a ‘business’ trip to Las Vegas.
https://www.gbnews.com/news/nhs-spending-work-trip-las-vegas
And more:
3. At the latest count, the NHS employed around 800 DIE (Diversity, Inclusion and Equality) staff. The direct salary cost is estimated at £40million a year, but when you take account of other employment costs – the real cost of the NHS’s DIE colossus is easily over £100million a year.
https://www.conservativewoman.co.uk/never-mind-patient-care-diversity-is-top-of-the-nhs-list/
I suppose that freedom of speech and diversity of professional opinion are not among the values protected by DIE.
Isn’t it odd that “Diversity, Inclusion, and Equality” requires a mixture of people with different skin colour, hair type, and culture; but absolutely forbids the slightest diversity of thinking?
Sorry for the repetition. I was fooled (I think) by the delay in publishing the first comment.
Love your comments, Prudence Kitten – Touche’
They haven’t got to that chapter in their indoctrination yet…
Interesting, my wife has just spent 40 – 60 minutes filling in a NHS form for an examination she is going to have. A lot of the questions are yes or no, no room for don’t know.
I fired my internist when he became obsessed with clicking boxes instead of practicing medicine.
I hope your troubles with the NHS resolve so you can go back to focusing on your enlightened take on CVD.
@JDPatten
I’m convinced that CVD is a thrombotic disease. The interesting thing about Lp(a) is it looks like a form of plasmagen – produces hard to remove clots.
Everyone has some Lp(a) – with that in mind – what they didn’t look for and didn’t tell us: is that the LDL found in plaque was not differentiated from Lp(a).
So pressure/tubulence stressed blood vesseles get micro tears – clots form – they get paved over with new intima – the clot now is called plaque. Rinse and repeat – layers on layer of this narrow the arteries.
What most cardiologist don’t know is that the coronary arteries are subjected to TWO pressure waves – one from the normal pulse – and a backward one forced out of the heart muscle as it contracts. Where these waves coincide in the arteries – you get very high pressure differentials. Sort of like water hammer..
I’m convinced that CVD is a thrombotic disease – focusing on lipoprotiens has not helped move the art forward.
I’ve looked at a lot of papers – no one seems to be concerned that they are conflating LDL with Lp(a).
One intervention – intermittent fasting should provide a period of low insulin – insulin – while it has effects on blood glucose – it has MANY other effects – and it shuts down apitosis – slows the removal of blood clots! You don’t want chronically elevated insulin.
Thank you, Irak, for your response.
With respect to the interesting notion of a water hammer: is this a proven notion? It’s been my understanding that, in the context of vigorous activity – the sort that would be causing damaging endothelial stresses – the smaller coronary vessels within the myocardium are squeezed closed during systole and are supplied their pulse of blood from the elastically filled major coronary arteries without the myocardium only upon diastole.
No?
What was the outcome of the libel trial? All that publicity and complete silence on the outcome.
There is no outcome yet
The wheels of British justice grind exceedingly slow. Julian Assange, for instance, has been locked up in Belmarsh high security prison for nearly 5 years now, without any charge being laid against him under UK law, while his lawyers try to prevent his extradition to the USA where he would very likely die in some way or other. Meanwhile every hearing, every rejected appeal, means another 6 months or so in that ghastly dungeon – for a man who has never even been accused of a crime under UK law other than fleeing to avoid immediate exradtion (and probable death).
There is a very old saying, “Justice delayed is justice denied”. Apparently British judges and lawyers have never heard of it.
What’s wrong with the NHS ?
The NHS is to introduce electric ambulances, raising concerns that its drive for Net Zero is being put above patient safety owing to the limited range and long charging times. A pilot scheme found the ambulances took up to four hours to charge and travelled an average of 70 miles between charging.
NHS England has set up a Greener NHS team with a combined salary bill of £3 million a year, leaked documents reveal. Officials created 48 roles, including five and six-figure salaries, as part of efforts to pursue an environmental agenda which means every medicine and product has to undergo an “evergreen assessment”. ** The 135-question process ** means that no decision can be taken without a product’s social values and contribution to emissions targets being considered.
https://dailysceptic.org/2024/03/15/fears-for-patients-as-nhs-introduces-electric-ambulances-in-net-zero-drive/
The NHS the way it is right now sounds like something right out of Terry Gilliam’s 1985 movie <i>Brazil</i>.