Stress/strain
When I started looking at cardiovascular disease I wondered why French people suffered far less than the Scots. I concluded, somewhat prematurely, that it was because the French ate food in a completely different way. They ate slowly, with the family, and food was an important part of life. Whereas, in Scotland, food was to be endured, not enjoyed. As scientific proof I would present Bovril and mince pie, at half time, at a Scottish football match.
When the French ate it was slowly, in a relaxed fashion. This allowed all the stress hormones, and all the nervous system involved in ‘flight or fight’ to settle down. So the French could digest and absorb food properly. Sugar levels would not spike; insulin would not spike. We would not have a battleground of cortisol and glucagon vs. insulin, and suchlike. Many animals after they have eaten simply find somewhere to go to sleep, to digest. Many humans just keep rushing about. Fast food indeed.
This brought me to led me to look at the overall concept of ‘stress’ in far more detail. Years and years later I have emerged – at times more confused than when I started. In the process I have fully embraced Einstein’s view that ‘Not everything that counts can be counted, and not everything that can be counted counts.’ I prefer it in the version. ‘Most things that can be measured don’t matter, and most things that matter cannot be measured.’ At one point this was my screensaver.
Stress fits well into this view of measurment. Stress certainly exists. Or perhaps to be more accurate ‘strain’ exists. In fact, both things exist, but measuring them… well, that it a trickier task. Which is one reason why medicine, obsessed as it is with ‘that which can be easily measured’, has tended to dismiss stress as a cause of anything. Focussing instead on blood pressure and cholesterol levels and blood sugar levels, and suchlike.
One thing I think I need to add at this point is to say that people do not actually suffer from stress, they suffer from strain. A subtle, but important difference. In that, two people can suffer exactly the same stress/stressor, yet react completely differently. One may feel strain, the other may not.
If, for example, two people are asked to stand up in front on an audience and give a talk. One person may dread this, the other may love the opportunity. They are both exposed to precisely same stressor, but the strains on the individual are diametrically opposed.
Extending this thinking somewhat, it became clear that stress, if indeed we should use this word at all, needs to be differentiated into, at least, four parts.
- Positive stressor
- Negative stressor
- Positive strain
- Negative strain
Of course, it gets even more complicated than this. We have short term and long term stressors. We have individual resilience, and suchlike. A person feeling strong fit and well may deal with a stressor well one day, yet when feeling physically ill, may be unable to cope with exactly the same stressor.
What mattered, I came to recognise, was not to get hung up on individual stressors, but to look at how the body adapts to different forms of external stress. It is impossible to look at someone’s lifestyle and say ‘they must under huge stress.’ Well, maybe they are, but maybe they treat it all in a positive way and it has beneficial effects on them.
I remember a cardiologist reviewing a lady who lived in the countryside, surrounded by a flower filled garden, with no money worries etc. He remarked ‘Well, stress obviously cannot have contributed to her heart attack.’ I merely nodded and thought to myself. ‘How can you possibly know? Perhaps her husband is horrible to her every day, and bullies her. Perhaps she yearns for another life.’
Of course, if you cannot measure strain, then the discussion does become rather pointless. ‘Anyone who has heart disease must suffer from strain, because strain is the cause of cardiovascular disease.’ This would be one of Popper’s circular arguments. A statement that relies on itself to prove itself. Similar to the argument used when a young person, with no traditional risk factors for heart disease has a heart attack. ‘Oh, it must be genetic.’
‘How do you know it is genetic?’
‘Well, they have no risk factors, and had a heart attack, so it must be genetic.’
Yes, indeed, it must be genetic… not. Try again, you idiot.
So, my attention inevitably became drawn to two researchers. Sapolsky and Bjorntorp. Sapolsky has studied baboons for many, many, years. He found that Baboons were pretty similar to humans in social structures, also in being perfectly horrible to each other, battling to gain higher status, bullying weaker members, and suchlike.
However, life in a Baboon troop normally muddles along quite well, but when the social hierarchy is disrupted by a new alpha male trying to take control of the group, there is a massive rise in cortisol levels, and a subsequent fall in white blood cells in all the baboons. Both of these are very significant signs of strain. You can look up Sapolsky on Google, he is a very entertaining lecturer and writer. His best known book is ‘Why Zebras don’t get ulcers.’
But, of course, Baboons are baboons. Humans are humans. Which is where Bjorntorp comes in. He wanted to know If strain, in humans, could be measured objectively [He called strain stress – as does everyone except me]. He found that it could indeed be measured by looking for a dysfunction of the Hypothalamic Pituitary Adrenal axis (the HPA-axis).
The HPA-axis is an extraordinarily complex physiological system that co-ordinates our responses to external stimuli – both negative and positive. If a lion were to walk into your room, right now, the HPA-axis would do its thing, and trigger the flight or fight response. [I would recommend flight]
The main hormones involved in flight and fight are: cortisol, glucagon, adrenaline (epinephrine) and growth hormone. The sympathetic nervous system response acts alongside the hormones. In a situation that triggers fear, the sympathetic nervous system lights up. This raise heart rate, pushes blood to muscles, and suchlike. Of course, at the same time, the stress hormones make the blood hyper-coagulable (far more likely to clot). You don’t want to bleed in a fight.
Anyway, Bjorntorp decided to measure twenty-four-hour cortisol secretion, in different populations. By this I mean he looked at what happened to cortisol levels every hour (or half hour) during the day. A normal cortisol secretion rises in the morning, goes down, rises at lunch, goes down and up quite a lot for the rest of the day. It is, basically, flexible.
An unhealthy cortisol secretion is more of a flat line. It does not peak in the morning, then it does not fall so much. He described this pattern as a ‘burnt-out’ HPA-axis. The hypothesis being that if someone is exposed to repeated activation of the HPA-axis it eventually becomes unable to cope. The system becomes damaged/inflexible.
This is similar to many other conditions whereby a ‘flattening out’ of normal responsiveness is a sign of significant physiological damage. [See under fetal heart monitoring, or the final development of type 2 diabetes].
As a quick aside, I should add that [inevitably and depressingly], a number or researchers have decided to measure cortisol levels in the morning to look for signs of stress/strain. They found a low level, in those with cardiovascular disease, and concluded that stress has nothing to do with cardiovascular disease, because the people they looked at had low morning cortisol levels. Ho hum.
Back to Bjorntorp. Here is the abstract from his paper ‘The metabolic syndrome–a neuroendocrine disorder?’
‘Central obesity is a powerful predictor for disease. By utilizing salivary cortisol measurements throughout the day, it has now been possible to show on a population basis that perceived stress-related cortisol secretion frequently is elevated in this condition. This is followed by insulin resistance, central accumulation of body fat, dyslipidaemia and hypertension (the metabolic syndrome).
Socio-economic and psychosocial handicaps are probably central inducers of hyperactivity of the hypothalamic-pituitary adrenal (HPA) axis. Alcohol, smoking and traits of psychiatric disease are also involved. In a minor part of the population a dysregulated, depressed function of the HPA axis is present, associated with low secretion of sex steroid and growth hormones, and increased activity of the sympathetic nervous system.
This condition is followed by consistent abnormalities indicating the metabolic syndrome. Such ‘burned-out’ function of the HPA axis has previously been seen in subjects exposed to environmental stress of long duration. The feedback control of the HPA axis by central glucocorticoid receptors (GR) seems inefficient, associated with a polymorphism in the 5′ end of the GR gene locus. Homozygotes constitute about 14% of Swedish men (women to be examined). Such men have a poorly controlled cortisol secretion, abdominal obesity, insulin resistance and hypertension.
Furthermore, polymorphisms have been identified in the regulatory domain of the GR gene that are associated with elevated cortisol secretion; polymorphisms in dopamine and leptin receptor genes are associated with sympathetic nervous system activity, with elevated and low blood pressure, respectively. These results suggest a complex neuroendocrine background to the metabolic syndrome, where the kinetics of the regulation of the HPA axis play a central role.’ 1
In short. If you are exposed to constant negative stressors, you are likely to burn out your HPA-axis, you will end up with abnormal cortisol secretion, and suchlike. You will then develop central obesity, high blood pressure, high VLDL levels, low HDL levels, high levels of fibrinogen, and many other clotting factors.
For those of you who have been paying attention to this series up to now. All of these things will increase endothelial damage, stimulate blood clotting and impair the repair systems.
For many years I knew that ‘stress’ was a very important factor in increasing CVD risk. All the evidence supported this, no evidence (other than people who failed to understand how strain affects cortisol secretion in the morning) contradicted it.
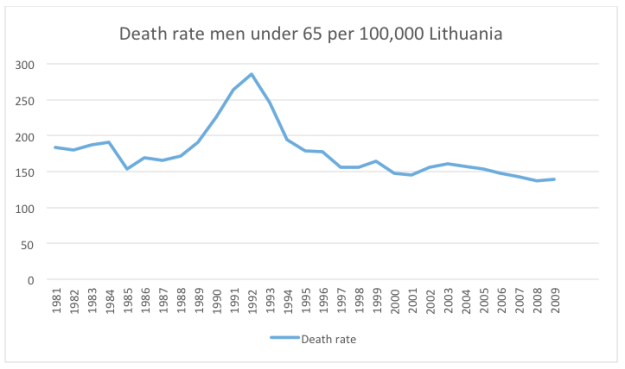
Which is where I return to my earlier graph on the rate of CHD in Lithuania in men under 65. As you can see, it was falling from 1981 to 1989, at which point it spiked, returning to its point of decline about eight years later.
Exactly the same pattern can be seen in Latvia

Here, I think we see Sapolsky’s work on Baboons, mirrored in humans, and mirrored in two countries that lie side by side, next to Russia. In 1989 the Berlin wall fell, the Soviet Union collapsed, the established social hierarchies disintegrated. Strain rose dramatically, and so did the rate of CHD.
This affected various Soviet Union states in slightly different ways. Poland, which had gone through the strikes and the battles of Solidarity years earlier, was very little affected in 1989, but the same basic pattern can be seen. In Belarus CHD skyrocketed, and has stayed very high [Belarus is the only dictatorship left in Europe]. In 1981 the rate of CHD in Belarus was 137/100,000 per year. In 2009, the last year with published data, it was 213. The Ukraine, and Russia also remain very high, both at 186.
During the same period, in Western Europe, absolutely nothing happened to CHD rates other than a slow and steady decline in all countries, year on year. The UK has gone from 143 to 33. Austria 83 to 29. Italy 62 to 19. France 39 to 15 etc.
I do not wish to hark back to a subject that I have previously covered. However, I can think of no other possible explanation for the rise in CHD in all ex-soviet countries after 1989 than the fact that there was a tremendous social upheaval, creating enormous strain. This signal is extremely strong and the data are remarkably consistent.
Data that links the work of Sapolsky and Bjorntorp who, in my opinion, ought to be recognised as the man who established, beyond doubt, how negative stressors can create measurable dysfunction of the HPA-axis which leads, in turn, to the metabolic problems that cause CHD. Or, to put it more simply. How stress causes heart disease. [No, it is not the only cause, but it is probably the most important single cause].

I love this man. he writes in a style I find comprehensible AND entertaining. Unfortunately I’m living proof that his theories are correct.
Sue, that was my first thought–he told my story, with anxiety pushing everything. What a relief to hear the unified conecept that makes sense of this mess.
As was my own mother. In fact I think she would have been a textbook case for Dr Kendrick! With very poor coping skills emotionally she developed CHD in her early sixties, had a triple by-pass op. and was always on medication of one sort or another. Stress/strain never left her so the NHS kept her going until her early eighties when the extra strain induced by my father’s final illness ‘got’ her and she succumbed to a cancer which killed her in thirteen months flat.
With stress being clearly implicated, it will be interesting to see if Europe “spikes” following the recent chaos. Syria and Iraq should be off the charts!
Unfortunately, from a research point of view, most countries that undergo enormous chaos, war, and suchlike – tend not to record medical statistics with any great accuracy. Croatia, Serbia, Bosnia Herzogovnia… big gaps. Slovenia, no spikes, data starts in 1985.
Post-Brexit Britain – different by region? I wonder? And would the HPA axis readings be different by socio-economic group? I guess so.
Something else to recognise about stress is that being ill is a strain on the body. I have m.e I also have flatlined cortisol taken via saliva tests, I am not mentally stressed, even by being ill I’m pretty steady and accepting on the whole, however something is wrong in my body. Loads of other markers are out, thyroid, liver alt, mitochondria ATP. Causes or symptoms? After studying myself for five years I’ve come to the conclusion that it’s not my rubbish cortisol levels and t3 conversion etc that are making me ill, so much as a signifier that something is placing strain on my body and in the process stressing all these things. But then as we all know it’s all my head according to the NHS and NICE, so what do I know?
A worry, isn’t it? I have a lot going on – some of which I’m very young for – and imagine my stress is sky high.
It’s all good news to me 🙂
Very, very compelling argument, in my view. I look forward to learning more.
So interesting! When a member of our family was under inordinate stress/strain for a very long time his whole nervous system cracked up. We came across the work of Dr Linus Pauling and Dr Abram Hoffer and Dr Andrew Saul, and discovered that their recommended massive doses of vitamins, especially niacin and vit C actually worked to heal the nervous system, stop addiction, and allow complete recovery from a very severe state of illness, including irregular heart beat, high blood pressure, under-skin bruising and appalling panic attacks amounting to severe anxiety disorder, and alcohol abuse started by needing to assuage the anxiety somehow or other. It seems, from our own mere anecdotal case history, that severe strain causes severe illness, including CVD, and that such sufferers are deficient in vitamins and possibly other nutrients such as magnesium, and that replacing these used up necessities can actually enable healing. If that works for many people, as those doctors found, (and it did for us) it could follow that it might work for many people under severe strain, possibly even used preventitively, adding hope for many victims of CVD and other manifestations of PTSD, could it not? Such mega-vitamin treatment might even help sufferers damaged by statins, when I suspect vit D is also very important, as statins seem to stop D being made and used by the mevalonate pathway. Thank you again, Dr K, for enlightening us at such length, and for all the research you do. Being able to quote references has enabled many sceptics to become “Kendrick Believers”!
Dr Kendrick would you accept a complementary copy of a book by another Doctor who worked in this field? please e mail me
So the booze, which leads to higher HDL, might in fact make you clot?
Bob:
Intermediate HDL Cholesterol Levels May Be Best for Longevity
http://www.newswise.com/articles/view/658581/?sc=mwhn&utm_content=buffer1e2f0&utm_medium=social&utm_source=twitter.com&utm_campaign=buffer
Today on the news was the statement that mortality from cardiac disease had reduced but incidence (morbidity) had increased. In short this means that preventive advice and therapy is failing but post-event therapy is improving which would seem to support the current use of stents. Statins may aid but when only one patien in 300 treated is actually “saved” per annum one wonders at the actual contribution they make to the overall reduction in mortality given their adverse reaction rate.
Three points I would like to raise:
1) Back in 1987 Anderson et al (JAMA 1987;257:2176-80) made the following comment in the abstract of their paper
There is a direct association between falling cholesterol levels over the first 14 years and mortality over the following 18 years (11% overall and 14% CVD death rate increase per 1 mg/dL per year drop in cholesterol levels).
Obviously to put that in the abstract means that they consider it to be very important.
2) I must also refer to a WHO-BHF graph
Mean total cholesterol, men(mg/dl), 2005. Source: BHF-HEARTSTATS
Estimated lowest mortality rates for TC blood levels
All Cause mortality 222 mg/dl 5.75 mmol/L
Non-communicable disease 210 mg/dl 5.49 mmol/L
Cardiac Disease 208 mg/dl 5.44 mmol/L
http://www.heartstats.org/documents/download.asp?nodeib=6797 This URL no longer exists? WHY?
Now on https://renegadewellness.files.wordpress.com/2011/02/cholesterol-mortality-chart.pdf
http://healthcorrelator.blogspot.co.uk/2009/12/total-cholesterol-and-cardiovascular.html
Clearly this and Anderson’s finding suggest that current advice to reduce cholesterol may be seriously flawed.
3) On top of this is the serious adverse reactions induced by statins, particularly in muscles and in active muscles as in athletes. Now cardiac muscle is always active. Yet when the US CDC and NHBLI announced an epidemic of congestive heart failure (CHF) the web page (like the WHO-BHFone) it was rapidly removed. It can now be seen at:
https://wayback.archive-it.org/3635/20130901052131/http://library.thinkquest.org/27533/facts.html
I have never seen the end of an epidemic on the rise. Epidemics rise, peak and then fall, as indeed cardiac mortality has done. In this case the rise of CHF was in lock step with increasing sales of cholesterol lowering drugs. It is also well known that the revolving door system between the US federal agencies and Big Pharma is well known.
Problem: can anyone really trust the authorities with their advice?
Also, 99% of stenting is in primary prevention.
Simple, if they die of something other than MI, it does not count towards CVD mortality.
Thank you.
Great! I was waiting for this post on `stress`.
Carlos Monteiro pointed to this is his work, talking about the autonomous nervous system, more specifically the sympathic nervous system. Also relating it to the PH level or acidity of your tissues. Described in his `Acidity Theory of Atherosclerosis`.
Makes sense.
Last week, I had a final meeting with a diabetes/endoctrine consultant at a leading London hospital, after stopping statins in March of 2015. So over the past year I was seen by a steady stream of medical people, all bent on getting me back on statins (to no avail).
At the final meeting the consultant was adamant that statins would prolong my life (I took them for about 3 yrs), but couldn’t tell me by how much and when I asked him for proof, he printed out a 2005 study entitled ‘Efficacy and safety of cholesterol-lowering treatment: prospective meta-analysis of data from 90 056 participants in 14 randomised trials of statins’. It was published in the Lancet and was authored (I assume) by the Clinical Trial Service Unit in Oxford (ctsu.ox.ac.uk).
When I queried him as to the source, he told me 50% of the data came from the drug manufacturers. In any case, it’s 12 pages of dense and complex data inc. graphs, and cites dozens of sources.
Toward the very end of piece, under the sub-hed ‘Implications’, we read:
My last readings in March of 2016 for my total cholesterol (without taking any CH lowering drugs, were overall 5.8, LDL 3.84, HDL 1.55). He considered it too high and wants to see it nearer to 4. I had another test that same day but still await the results.
There’s no doubt that taking statins in sufficient quantities does lower cholesterol (after coming out of hospital after my heart attack, my total was nearer to 1 but I was on a massive dose!). So is the claim that statins reduce my chances of having another heart attack by one-third, borne out by the facts? The key seems to be the 5 year period after the attack.
I don’t know what to make of this (it’s 4 1/2 yrs since mine).
Barb,
Check this out. There are VERY few that get any benefit from statins and no way to know who it might be.
http://www.drjohnm.org/2016/03/a-new-way-to-discuss-statin-drugs/
Check this out. There are VERY few that get any benefit from statins and no way to know who it might be.
The 7% who do gain from taking statins, appear to get an ‘extra’ 99 months of living. In other words, it’s pretty much a random event, if you don’t know who or really how long (longer than what?) you’ll actually get.
But is there a corresponding graph for a similar set of people who didn’t take a statin, I wonder? Would the results be any different?
+Barbrovsky . . . the numbers needed to treat (NNT) is what you need to ask about; that is, the number of people needed to take statins of 1 to be not suffer a fatal coronary in a given time (usually 5 years). Taken from the NNT site (worth a look) they give, for some one with confirmed heart disease, over 5 years and NNT of 1 in 83. So . . . ONE person in 83 is predicted to be saved by statins within the 5 years. . . the other 82 will succumb.
Imagine that of 1000 people with CVD/iHD 83 of them would be predicted to succumb to a heart attack with in the 5 years (Just under 10%). . . but if the 83 had taken statins . . . one would have been saved and could go on to join the other 917 who did not have a heart attack.
The trick as I see it is to look for something with better odds than 1:83 that gets me in to the 917 group. Exercise, meditation, mindfulness, plenty of vegetables, keep a check on the weight (sorry Dr Kendrick had a meme attack), keep those peaking glucose levels down, keep the triglycerides down, cut the crisps and the beer.
I do hope you held out. I do not know your age, but remember there are many studies that show that for older people there is an positive relationship between longevity and TC. At 66 I am ok with my TC 6.4mmol/l and HDL 1.5mmol/l.
(Really should find an estimate of what percentage of people with heart disease succumb to heat attack over 5 years – I am assuming about 10% – More exactly 83/1000=8.3%)
Antony Sanderson:
Nope, I’m still not taking statins. BTW, my last test for cholesterol showed as having a total level of 4.9. It seems that after five years it might be my stents that could create a problem not my cholesterol, according to the ‘consultant’. Cheerful buggers aren’t they. Well five years since my heart attack/stents comes up in a couple of months.
As to all the stats? It’s pointless even considering them, after all I’m NOT a statistic.
Good question! Is it something THEY would think to ask?
Thanks for a most interesting Part XX! I just finished reading the book “The Power Paradox” by Dacher Keltner. The author spent much of the book explaining why less-advantaged, lower income folks in Western society have lower life expectancy and higher rates of CHD, cancer, Type 2 diabetes, and obesity than those in the middle-to-upper-income group. His conclusions are the same as yours — that the many stressors in their lives, such as food insecurity, financial problems, feelings of political powerlessness, etc., are negative take their toll on the HPA axis to create the ideal conditions for these illnesses. He notes that some of the things that “conventional wisdom” would see as stressors in high-income, successful people — long hours at work, pushing for even more success, dealing with large budgets — are often perceived by the successful “stressee” as positive challenges, and thus not deleterious to their health.
I have often said that it seems as though movie stars lives longer than the average joe (or at least the great majority of them) and that it’s because they usually don’t have financial woes, which is the hinge to a lot of other woes the general public has to deal with. Nowadays, it’s the same with most politicians.
So, cortisol has a lot to do with central obesity? I mean, is there a way to control or get the body to regulate cortisol? I deal with central obesity even though we eat (and always have) the way most people who buy local or grow their own food do, and we buy pastured meats as much as possible, use real home-rendered lard, etc. (Much the same as the WAPF recommends for people to eat). Never really believed in that cholesterol nonsense and certainly never ate low-fat junk. I do have a bit of a sweet tooth but well controlled in the big picture of things. I’ve been told that cortisol levels might be the reason for my constant struggle with central flab that simply will not go away no matter what I do. Any thoughts on “fixing” the cortisol issue (which seems to be responsible for several issues including adrenal, as well)?
Thanks for writing this series. Much great information, and I hope more to come!
Sundancer, you didn’t mention what your intake of carbs is per day. Are you under 50 g? You also did not mention what your blood glucose level is 3 hours after eating a meal that might be high in carbs. Obesity has a lot to do with insulin resistance primarily. So you have to be sure that you are consuming a very low level of carbs before you start looking for other causes, especially if your blood glucose is not down to baseline level within about 3 hours after a meal.
Great stuff doctorK
Thank you
Great input as always!
My own CHD case record is a clear proof of the importance of negative stress and which was also the only “cause” the “experts” could find. Yesterday I had a long talk with a ten year younger former colleague of mine, still working, who recently had a heart attack and he confirmed that the stress factor was obvious also in his case.
Today I still wonder why I survived and feel fine today. The only thing I can come up with is that I actually took control of my own destiny and then worked with at broad brush. I think it is well established that stress levels decrease when you actively work to solve your problems.
Control = good. Loss of control = bad
“Bovril and mince pie”
Okay, I had to look that one up.
And if it isn’t a cause of CVD in Scotland, it should be!
Actually, while reading the new installment yesterday, I wondered if the Scots felt / still feel more strain realative to the English or continental Europeans.
Is it vestiges of Calvinism? Just some armchair philosophizing here: Scots are generally good business people, but that would likely constitute positive stress. Also, there are still a lot of Calvinist values in the Netherlands, hidden below an easiy-going and tolerant surface, and that does not seem to raise CVD.
Is it the disadvantaged in Scotland who are more stressed? My impression was that Scotland was more inclined towards Social Democratic politcs than England.
How does this fit into the big picure?
I think that the clearing out of the tenements in Glasgow resulted in a very high rate of CVD for many years afterwards. Half a million people shifted from, pretty horrible buildings, to the lovely high rise flats. Now, thankfully, demolished. General message… pull apart communities and families and watch them die. [See under Australian aboriginals].
Yes, but this was not being done all over the country, at a rate big enough to drive the CVD rate up by nearly a factor of two compared to England.
WASHINGTON (Mar 24, 2016) –
New research shows that individuals with a greater degree of activity in the stress center of the brain also have more evidence of inflammation in their arteries and were at higher risk for cardiovascular events, including heart attack, stroke and death, according to a study scheduled for presentation at the American College of Cardiology’s 65th Annual Scientific Session.
While there has been mounting evidence of the strong link between stress and heart disease, relatively little is understood about the mechanisms behind this stress response and what might put someone at risk for cardiovascular disease. This is the first study to use medical imaging to show a possible association between biochemical activity in the brain and arterial inflammation. Arterial inflammation is a key component of atherosclerotic disease—the buildup of plaque in the artery walls that restricts blood flow through the body and is highly predictive of future cardiovascular events and stroke.
“Our study illuminates, for the first time, a relationship between activation of neural tissues—those associated with fear and stress—and subsequent heart disease events,” said Ahmed Tawakol, M.D., co-director of the cardiac MR PET CT program at Massachusetts General Hospital and co-author of the study. “There is a need to develop greater knowledge in terms of the mechanism that translates stress into cardiovascular disease risk, given the prevalence and potency of stress as a risk factor.”
Data show the more activity occurring in the amygdala—the stress center of the brain—the more inflammation patients had in their arteries and the greater the likelihood of having cardiovascular events. There was also a corresponding activation of the bone marrow. Bone marrow releases immune cells called monocytes that can trigger inflammation in other parts of the body.
Researchers examined PET/CT scans for 293 patients (average age of 55 years) who originally received the test between 2005 and 2008 for cancer evaluation but were found to be free of active disease. The scans allowed researchers to objectively measure activity in regions of the brain, as well as the bone marrow and arteries. Patients were excluded if they had evidence of cancer, established cardiovascular disease or were younger than 30 years old. An hour before the scan, patients were injected with a radioactive atom attached to a glucose molecule as a tracer; tissues that were more active would metabolize more of the glucose and glow more brightly on the scan. A radiologist who had no knowledge of the patient’s history or identifying characteristics measured the images. Activity in the amygdala was compared to other regions in the brain. Researchers then grouped patients based on the relative magnitude of brain stress activity.
After correcting for age, gender and other cardiovascular risk factors using the Framingham Risk Score, there was a 14-fold greater risk of cardiovascular events for every unit increase in measured brain stress activity. Over the approximately five-year study period, 35 percent of the patients in the high stress center activity group later suffered a cardiovascular event, compared to just 5 percent of the low stress center activity group.
The researchers further observed that activation of the brain’s fear centers, bone marrow activation and arterial inflammation may together contribute to a mechanism that provokes cardiovascular events. Tawakol said this points to the need for future studies to test whether interrupting this mechanism reduces the burden of cardiovascular disease associated with stress.
“Over the past several years, it’s become clear that stress is not only a result of adversity but may itself also be an important cause of disease. The risks of heart disease linked to stress is on par with that for smoking, high blood pressure, high cholesterol and diabetes, yet relatively little is done to address this risk compared to other risk factors,” Tawakol said. “We are hopeful studies like this bring us closer to understanding how stress may lead to heart disease.”
While researchers were able to objectively measure stress activity in the brain, the retrospective nature of the study meant that they could not compare it to subjective measures of patients’ stress levels. Additionally, the patient population is limited to individuals who received PET/CT scans to screen for cancer.
Still, Tawakol said the study findings prompt the question of whether treating stress and reducing the activation of the fear center of the brain may lead to less atherosclerotic inflammation and, ultimately, reduce cardiovascular events. Larger prospective studies are needed.
– See more at: http://www.acc.org/about-acc/press-releases/2016/03/25/09/43/signs-of-stress-in-the-brain-may-signal-future-heart-trouble#sthash.O4SIigK4.dpuf
Errett
Thanks very much for the link. It would seem to provide hard evidence in support of Dr Kendrick’s hypothesis that cardiac disease is closely associated with stress/strain. An old saying of course was “He/she died of a broken heart”. I must try and get a reprint
Dear Dr Kendrick
You email reminds me of a report I saw on the MAOA gene variants, an outcome of a large lifetime populations study originating in Dunedin New Zealand. This gene seems to be associated with responses to stressors, in some it is dubbed the short fused gene.
e.g
Candidate genes for aggression and antisocial behavior: a meta-analysis of association studies of the 5HTTLPR and MAOA-uVNTR.
Ficks CA, Waldman ID.
Behav Genet. 2014 Sep;44(5):427-44. doi: 10.1007/s10519-014-9661-y. Epub 2014 Jun 6.
PMID: 24902785
A regulatory polymorphism of the monoamine oxidase-A gene may be associated with variability in aggression, impulsivity, and central nervous system serotonergic responsivity.
Manuck SB, Flory JD, Ferrell RE, Mann JJ, Muldoon MF.
Psychiatry Res. 2000 Jul 24;95(1):9-23.
PMID: 10904119
There was a series of 4TV documentaries on TVNZ a couple of months ago which may still be avialable on line. Episode 3 is the one of interest
https://www.tvnz.co.nz/ondemand/why-am-i/23-05-2016/series-2015-episode-3
Regards
Adrian
[https://www.tvnz.co.nz/etc/designs/ondemand/images/bg_loading.gif]
Watch Why Am I? – Episode 3 – TVNZ OnDemand http://www.tvnz.co.nz What determines our personality, health, wealth and happiness? In 1972 the Otago University Medical School embarked on the ultimate nature/nurture test, to study 1037 …
________________________________
I got a couple of paragraphs in and said to myself, ” this sounds like Sapolsky and his zebra book. I must bring it to Malcolm’s attention in the comments”. LOL! You got there before me! Sapolsky has a whole series of lectures (25 from memory) on You Tube, if anyone’s interested. Great stuff….a whole course in human biology.
Fascinating! I wonder how, and why, some stresses strengthen us, whilst others are deleterious?
I think it may have something to do with the type of stressor and the duration. So, if you are preparing for an important presentation or a deal, or a wedding, then it tends to be relatively short-term stress and it is to some extend under your control. If on the other hand you have a disabled child or long-term sick parents, get made redundant, live on an awful estate, then that is long-term strain that you have almost no control over.
And if you are the sick relative, especially long term sick, I guess.
The distinction between stress and strain is present in engineering. Stress is the load on the system and strain is the response of the system to the load. The issue is then how to reduce the strain and help the body regenerate from it fully. When people are given some simple training they can learn to sense their level of strain and intervene with non-pharmacologic methods much earlier and more effectively. I put together some material on this which was used in an article on the stress that sales managers face. So this idea has a very broad application.
What we pay attention to and how we breathe have a huge influence on the HPA axis. Interestingly both of those, attention and breathing, are the focus of a lot of meditation techniques and not surprisingly those tend to reduce the effects of stress, probably by reducing certain types of strain.
The techniques that are most useful include:
-Techniques to recover from strain quickly and practice those daily. Herbert Benson’s “Relaxation Response” is a simple and effective example.
-Techniques to experience stress with less strain. Note that this is not the same as toughing it out, it is more like Tai Chi where one remains relaxed while exerting effort. We need to make these a habit so we use these without thinking about them. Keeping the breath and shoulders soft when under pressure is an example.
-Techniques to avoid making external stresses greater than they are by misperceiving them or adding to them. For example, letting go of perfectionism. These techniques might be called “the ancient art of not making things worse.”
Great post.
Perhaps when we talk about stress and strain like this we are using an incomplete metaphor. Sometimes that is useful and sometimes it clouds the details. Usually when people talk about stress they mean distress. That concept puts the issues more to front and centre.
But … the material science stress analogy has more features that can be used to expand the metaphor: strain as you say can happen at different rates wrt applied pressures. Many people are changed by that strain; some are hardened, others buckle; some change disproportionately and will never be as resilient, they might reach their limit. And so on.
Is it a useful mental model to have though, can it lead to practical solutions and make testable predictions? Are people based on material science or is material science based on people? I’m not trying to be funny here rather attempting to describe how these big, apparently solid ideas are just labels for a huge set of interconnected processes and messy details and that the overarching idea can also be a limit.
Language is a cow sometimes.
I do not like to be self-serving. At the same time the book I co-authored on meditation has received excellent reviews for its clarity and helpfulness. Since these comments are moderated I will defer to Dr. Kendrick’s wisdom and let him decide whether to approve this. The book is Real Meditation in Minutes a Day, Wisdom Publications, 2008 and is available from the publisher and through the usual retail channels.
As I like the idea of meditation, and I think it can help people, I am happy to make people aware of your book.
Thank you Dr. Kendrick. I have been referring your work to a lot of my patients.
I’ve often thought that the main benefit of yoga is the relaxation/meditation at the end of each session.
A very interesting article. I had a completely unexpected heart attack 3 years ago at the age of 50 and am very strongly inclined to agree with your suggestion of negative strain/stress as the cause, though this has not been identified by my doctors – indeed, it’s not on their list of “likely factors”, presumably because (as you say) they don’t know how to measure it properly. I am, generally speaking, a fit and healthy male. I had a detailed health check about a year before my MI which gave me a clean bill of health except for somewhat high cholesterol levels (overall 6.1, LDL 4.6). I have never considered cholesterol to be the likely cause. My question is how to reduce the likelihood of a repetition? I’m someone who is (probably) overly self-conscious. I don’t sleep well (never did). I (perhaps) worry about things too much. I’m a regular alcohol drinker (couple or three glasses of wine most evenings) but from what I’ve read this is unlikely to have had much to do with my MI, and may (in the opinion of some) even be beneficial. Methinks I’ve inherited some of these characteristics from my mother, who is a classic “worrier”, but who is still very much around and healthy at 79. How do I change myself? Is it enough that I take my medicine – a daily baby aspirin, low dose of statin and beta-blocker, various supposedly heart-healthy supplements and exercise regularly? What else can I do? Thanks again for your blog.
Maybe the feeling of ‘not being in control’ affects men more adversely than it does women?
Before my severe MI i seldom had a glass of wine. Doing my homework, refraining from the comprehensive by-pass offered and ALL medications, my wife realised that a glass of wine a day could though be beneficial but after 17 years now, well and fine, I have suspected that alcohol, the only medicine I take, may be a poor sleeping “pill” since having a few glass I tended to wake up after a couple of hours of though good sleep. Now I have also abstained from this “medicine” for about a month and note a significant improvement.
Was it just a couple of hours? Or was it after the ‘first sleep’? See Ekirch’s fascinating work – it seems that, at least until late 17thC normal was ‘two sleeps’ per night (ca. 4 hrs, then a wakeful period, then another 3-4 hours sleep). First street lighting was late 17thC, then industrial revolution and now ‘everyone’ regards 7-8 hrs uninterrupted sleep as normal and people get stressed (and strained!?) if they wake after a ‘first sleep’. I seem to have reverted to the 16-17thC with my own sleep pattern (yes, after 2-3 glasses of wine with dinner)!
Peter – I decided to ‘own’ my body. It’s mine and my responsibility to keep it in good shape SO I ditched the aspirin and the vile statin because they were prescribed without my educated consent (and felt better without them within days) refused BP medication for moderately elevated BP because at the age of 74 I don’t expect to have the same flexibility, the smooth unlined skin etc. of a 20 year old so why should I expect to have the blood pressure of a 20 year old. Sadly despite following a HFLC diet it seems I still need my diabetic medication but I am careful of what I eat, test BG levels often as a means of taking control over something which it appears is to a greater or lesser degree controlling me (my grandmother, mother, brother, niece all had or have it)
Of course there are things which I can’t control – stress/strain doesn’t just appear on a macro level within society but on a more micro level within the family, within personal relationships, and it’s hard sometimes not to feel helpless, but by concentrating on what I CAN do I get by.
By the way, regarding sleep – I have starting wearing a sleeping mask at night and am now able to fall asleep quickly and enjoy 7 or 8 hours of good solid sleep. If you can bear the sound of the thumping of your heart earplugs are really good too. Nothing like a bit of sensory deprivation at night.
zzzzzzzzzzz
I bet you and your Mum “worry” in very different ways. Plus it’s not always a bad thing to have a good old worry with others. Problems shared etc. Not sharing worries is a different matter as they get bottled up which is bad.
Why don’t you have read of the book described by fellow contributor JPA. I know I’m going to as their comment made good sense to me.
I’m not what I would describe as a worrier but my stresses are caused by anxiety which I think is different. Almost “exam nerves” (for example looking at a BP machine). I can feel that “flight fright” kicking in. I’d like to find a useful technique to help calm that feeling (at the moment I generally use avoidance which is not always wise).
As Dr K said, control = good.
Thanks all for your comments. Regarding alcohol, I concede that I probably drink slightly more than most doctors would recommend. However, it is my only vice, I enjoy it and it relaxes me. Given the balance of probabilities judging by what I’ve read the amount I drink is only a slight negative health-wise, and one which I’m prepared to risk for the pleasure I derive from it. It is possible that I would sleep slightly better if I were teetotal, but I am I suspect “naturally” a poor sleeper. I remember in my teens, well before I drank alcohol, having trouble getting to sleep or waking and having trouble getting back to sleep. Nowadays I use zopiclone to assist on nights when I’m having trouble sleeping, and while not the perfect solution I find it the lesser of two evils.
Thanks for the suggestion, but I don’t think a sleeping mask would work for me.
Regarding JPS’s book on meditation – I bought it yesterday. Waiting for it to arrive by post.
Regarding dropping my prescribed meds, yes this is something I’ve thought about. I did stop taking the statins, but my cholesterol went back up and my doctor/s told me to go back to them. Although I’m fairly convinced cholesterol had nothing to do with my MI, I find it hard to go completely against my medical advice, although I did insist on the minimum dose, which apparently still provides the anti-coagulant effect – and which is why I still also take the baby aspirin. The beta-blocker I’m really not convinced I need. I never had high blood pressure. I’ll bring this up again when I see my doctor for the regular appointment, but I already know what he or she will say.
Yes, I’m sure my mum worries about different things than I do – about me for example, even though she knows nothing about my MI (it would make her worry even more). But many of our traits are similar. To be honest though, I am not a worrier like my mum is. I’m just a lousy sleeper. I recall being astonished by my friends at university who were able to sleep in until mid afternoon after a big night out, whereas I’d always wake up at the usual time. Or friends who can nod off in the afternoon almost at will. In my next life this is perhaps the talent I’d most like to have.
About meditation: check out http://www.dhamma.org
For those of you in UK, you have two large centers there. For those in other countries, they have them all over the world.
It does require taking 10 days to go and learn the technique but the results are well worth it, IMO.
Hello again Peter,
I think you’ve hit the nail on the head pointing out your sleep difficulties. But don’t worry about what others seem to do. My Dad could have slept on a washing line. Everybody is SO different. You sound like me – I can’t switch my brain off but I can’t lie in either as I get a headache.
My understanding is it’s not how much sleep you have but the quality of the hours that you do manage. So many restorative processes take place when the body is in a deep, relaxed state but unfortunately it needs to really be a natural one. Not drug/alcohol induced.
The trick with booze is to have just enough to relax you but not enough to knock you out.
There are also lots of techniques to help you actually nod off. I’m sure there will be something in the book you have ordered. Mindfulness, thinking about breathing etc – all makes good sense to me. The hard bit is practice, perseverance and not expecting it to work immediately. You probably have a lifetime of habits to change so it will take time.
Hopefully you’ll find the bedtime/sleep/waking pattern that is right for you.
I found this section of your mammoth and very interesting “book” of particular application to myself. Now in possession of two stents acquired a year ago. I have had my thyroid gland zapped with radio active iodine (2013) and am , of course, hypothyroid. As you are aware this is an affliction which is not treated at all well. I have been struggling for the last three years with weight gain etc. Probably caused by the beloved levothyroxine as I self treated for a while with NDT and lost weight but that was when the stents arrived. I am sure I am suffering metabolic probs. Thought you could include this in your research. There are thousands of us out here with this ill treated problem!! Now being accused of being ? diabetic!!
Janet
You may find some interesting things in a recent blog by Dr Duane Graveline.
https://www.spacedoc.com/articles/selenium-impact-of-statins
Selenium is an important element and a deficiency can cause a cardiomyopathy (Keshan disease). The selenoproteins are also involved in the thyroid.
I now eat three or four brazil nuts daily. (Not more! you can overdose on the selenium if you overdo.)
I started this after reading the research that found a reduced rate of atrial fibrillation following heart surgery when an infusion of selenium precedes the surgery.
It seems to help with my pesky PACs and PVCs. It’s nice to be less rhythmically challenged.
JD Patten
Do you have the reference to the AF response to selenium?
I have had to write several reports on selenium for veterinary product authorization over the years. It is also useful in piglet anaemia as well as severe muscle diseases in ruminants. I take a standard selenium supplement.
As far as I know selenium toxicity in humans was related to the beer industry. Certainly when I first got involved with selenium as a veterinary supplement it set the alarm bells ringing in the VMD.
Mikecawdery,
Here ya go:
http://www.ncbi.nlm.nih.gov/pubmed/27406157?dopt=Abstract
https://ods.od.nih.gov/factsheets/Selenium-HealthProfessional/
JDPatten
Many thanks for the links. This blog and its comments do help to expand knowledge
Another excellent post in this series Dr Kendrick, and after 12 years of reading and learning, I 100% agree with every word.
Love this series! Thank you.
very good
good
CVD numbers are declining in many western countries. Is this compatible with the stessor/strain hypothesis?
I blieve that it does, although this is somewhat difficult to prove beyond doubt. Of course, there are other factors at work. Less smoking, a reduction in pollution and the use of heavy metals such as lead in petrol, and suchlike. Also, one cannot overlook advnaces in mainstream medicine. Survival post-MI has greatly improved, and a certain number of the medications and interventions have been of benefit.
nice to know some treatments work. how about bp meds. are these beneficial
So, would physical stressors, like smoking and pollutions, work the same way as mental stressors when it comes to the HPA-axis response?
Smoking does create HPA-axis stimulation, but also has direct effects on clotting and the endothelium – as do pollutants
“this is somewhat difficult to prove beyond doubt”: not half. As you point out, the decline has been widespread, the decline of smoking and so forth rather erratic. A hae ma doots.
Recent political and economic instability in Europe would suggest an uptick in strain-related CVD. Any sign?
And the 2007-8 crash should have had an effect.
The figures I have certainly show a decrease in mortality but in an increase in morbidity based on a recent BHF spreadsheet. In short while morbidity goes up therapy improves so mortality decreases.
Let’s keep on reading the good work
Another interesting element relates to the Vitamin Ks. The “cure” for ARs is warfarin. I have been told that it is 4% – apparently good for medicine. Warfarin restricts Vit K1 but Vit K2 is derived from K1 and warfarin apparently increases vascular calcification. A Youtube presentation by Dr Bruce Ames explains.
Dr Ames is a real scientist (as distinct from some BP supporters)
So how would one insure that they have what they need in order to get off warfarin?
Having gone into the data I found that the probability warfarin benefit was better than aspirin only 1 in 40 patients. If one is tolerant to aspirin it is an option. Incidentally from the MHRA Daps records, warfarin is involved in more death reports than aspirin despite the huge difference in weight of drugs used in humans.
So one would have to suck it and see, tolerance wise.
The issue in this case is DVT, by the way.
Malcolm
You state in your closing paragraph “negative stressors can create measurable dysfunction of the HPA-axis which leads, in turn, to the metabolic problems that cause CHD”.
Would diet induced metabolic syndrome hook into the same process but after the HPA-axis?
I think that there is a difference between diet induced insulin resistnace and stressor induced insulin resistance.
Please, explain the difference.
Yes, please explain the difference as it is of utmost importance in my opinion. Because if, for example, eating junk foods put a strain on the hpa axis, why would the strain be different than being bullied, ignored by loved one, or having to relocate in war time.
I am curious about the steady decline in CVD in the West. Is it fair to say that the stress/strain that people are suffering has continued to decline over this period? I think I would have expected it to have levelled off (at least) after 1989, when capitalism was unleashed to cause problems – such as the export of jobs. I vaguely wonder if people are less stressed because they can be in contact with their friends so easily (I tend to leave my mobile switched off when I don’t need it).
“As a quick aside, I should add that [inevitably and depressingly], a number or researchers have decided to measure cortisol levels in the morning to look for signs of stress/strain. They found a low level, in those with cardiovascular disease, and concluded that stress has nothing to do with cardiovascular disease, because the people they looked at had low morning cortisol levels. Ho hum.”
This seems typical of modern science – take the measurements in such a way as to confirm the hypothesis that you most want!
Re cortisol testing question
I had my cardio vascular event back in April and it took 3 months and numerous attempts with my GP to get the following 2 of the 3 cortisol tests done:
(1) Blood suppression
(2) 24 hour urine
leaving
(3) Bjorntorp’s 24 hour testing
It’s my understanding that the 1st two tests don’t demonstrate the functionality of the HPA-axis and only proved my cortisol secretion was normal when the samples were collected, and thus don’t really help when trying to ascertain why i collapsed.
My question to the readers – after 3 months since my cardio vascular event, should I find the money for the 24 hour testing? By which I mean, after 3 months would any HPA-axis burnout be healed/corrected?
Thanks
While the mortality rate due to CVD is going down the incidence of cardiac disease is still going up. It seems that post-MI actual treatment is improving (Stents ??), preventive advice and therapy is not.
Mike,
As I pointed out to Mark Heller in the previous plog, I don’t think this is true:
Having read Malcolm’s books, I don’t think this is the case, and indeed, if you look at Figures 2.5a, 2.5b, and 2.6b in this link
Click to access bhf-trends-in-coronary-heart-disease.pdf
you will see that the rates of CVD have gone down – not just the mortality.
David
Try
https://www.bhf.org.uk/research/heart-statistics/heart-statistics-publications/cardiovascular-disease-statistics-2015
Check the mortality and morbidity (incidence) These spreadsheets can be down loaded
Mortality has certainly reduced but morbidity (Table 2a) due to CVD has gone up
Mike, I am a bit confused. The link you gave me did not seem to contain graphs relating to the trends in CVD morbidity over time, however, this link does:
Click to access bhf-trends-in-coronary-heart-disease01.pdf
Look for example at graph 2.6a or table 2.6. Both of these are ‘age standardised’ by which I assume they mean that a correction has been made for the fact that the age profile of the population has changed, and the incidence is quoted per 100,000 population.
The decrease seems quite definite! Perhaps Dr Kendrick can add something here?
There are many different graphs to be seen on the BHF site. From 1969 till now CHD rates have dropped five fold in the UK. In general death rates are per 100,000 per year. The ages are often separated out – in different ways in different countries. Males CHD rates in the UK in 1969 were 500 per 100,000 per year in those under 75. This has now dropped to 100 per 100,000 per year. This figures seems pretty robust.
Thanks Malcolm – I was fairly sure I’d got this story straight – the incidence of CVD has gone down massively over time – it isn’t about improvements in the care of people once they have CVD!
I can’t imagine what is still causing this reduction – unless it is some disease causing agent that is becoming less prevalent in the West. Surely stress levels must be on the rise again?
A disease causing agent that only affects people in the East, men more than women, aboriginals more than the surrounding population, diabetics more than non-diabetics, immigrants to the UK more than the native population? It would be interesting to speculate what this might be. A recent study in Greece showed rate of MI increasing.
In countries where stress levels more certainly are on the rise, the rate of CVD is rising. Two countries that I find I cannot explain are Somalia and Zimbabwe.
David
The url I provided leads to the following:
Downloads
This publication can be ordered in hardcopy through the BHF Orderline on 0870 600 6566, by email orderline@bhf.org.uk (quoting CVDSTATS15), or downloaded as a pdf.
All the charts and tables from the publication are available for download on this page:
Each of these *.xls spread sheets can be downloaded
Chapter One – Mortality (Excel)
Chapter Two – Morbidity (Excel) The important one in terms of incidence
Chapter Three – Treatment (Excel)
Chapter Four – Costs (Excel)
On Page 2.2a of the morbidity spreadsheet at the bottom you will find the following
Year 2010/11,2011/12,2012/13,2013/14
United Kingdom All diseases of the circulatory system (CVD), 920216, 932,352, 931211, 956757
This group is further divided if you are interested. It also provides information on the four nations of the UK. In all cases there is a rise in numbers from their start (2005/2006 in the case of England and Wales)
All four spreadsheets in red can be downloaded.
Hope this helps
Mike,
You quoted
“Year 2010/11,2011/12,2012/13,2013/14
United Kingdom All diseases of the circulatory system (CVD), 920216, 932,352, 931211, 956757”
However, surely what matters if you want to discuss the effectiveness of treatment is the age adjusted incidence divided by the population size! You have a growing population, and people may live longer but still die of CVD – everyone dies of something!
A few blogs back, Dr Kendrick explained how the various CVD risk calculators are pessimistic by a factor of five, and he explained that the reason was the steady decline in the magnitude of the problem!
Get ready. Here come the posts on yoga, meditation, and mindfulness! 🙂
Why go to all the trouble of yoga and meditation when there are plenty of pills available like Buspar, Prozac, Paxil, Effexor, and Vanatrip. Except…
Apr 6, 2011 New antidepressant warning – Prozac and other drugs raise risk of heart attack and stroke.
Mar 22, 2016 Prozac – Antidepressant with Serious Side Effects – Drugwatch.com
Apr 14, 2012 Antidepressants: This Best-Selling Drug Attacks Your Heart, Brain and Bones
Aug 17, 2009 There has been recorded cardiovascular (heart) side effects from Prozac
Mar 5, 2015 Popular Antidepressant Could Help Reverse Heart Failure
Dec 16, 2015 Antidepressants Linked to Lower Risks of Death and Heart Disease
Apr 6, 2011 Prozac and other drugs cause thick arteries, raise heart risk
What’s not to love? All three can increase GABA levels in the brain, reducing anxiety.
Dr Kendrick, I agree stress is the single greatest threat to health. However stress is itself a difficult topic to grasp and I’ve always found talk of “positive stressors” particularly obfuscatory. Moreover I can’t even begin to imagine any use for the term “positive strain”.
My own preferred terminology is to simply say that stress is condition of fear/worry when gluco-corticoid hormones are released at dangerous levels (detectable via blood tests). This terminology is simpler because no-one is ever going to interpret a condition of fear/worry as a positive, except only that it works exactly as evolution intended: the pounding heart gives you a better chance to fight/escape a dangerous predator.
In this simpler terminology it can be recognised that some people can climb a cliff-face without ropes and do so entirely without stress (fear). The majority of us would be quivering wrecks. If you love your job you can do an hour of overtime and gain extra enjoyment from doing so. Overtime is only a stressor to those who hate their jobs etc. In humans the relevant issue is whether the individual FEELS in control. How an individual FEELS in response to a given situation is down to a complex nexus starting with a positive upbringing by unconditionally supportive parents generating positive self-esteem, sustained afterwards in the wider world by a regular experience of success.
The reason I always bang on about Grossarth-Maticek is that his scientific experiment provides HOPE. It proves scientifically that psychological interventions can be designed which dramatically improve people’s health.
In my forthcoming book “The Egalitarian” I will argue that there is and always has been one purely human solution to the evolved condition of stress seen in baboons. Happiness, health, fairness and efficient organisations are all enhanced by egalitarian thinking. Any individual who loves their neighbour as themselves while perceiving their own value to be the same as that of their neighbour is firstly a boon to society and secondly a champion of their own health and happiness.
There was a carpenter about two thousand years ago, who recommended loving your neighbour as yourself. If only we did as he said, instead of getting bound up in ways to worship, let alone setting up inquisitions and killing people for stating the world is round when the authorities know it is flat, we would all have been free of a great deal of strain over the centuries. Still would work today, of course…
What great stuff in the last paragraph!
Nutr Metab Cardiovasc Dis. 2016 May 28. pii: S0939-4753(16)30079-5. doi: 10.1016/j.numecd.2016.05.008. [Epub ahead of print]
Role of endoplasmic reticulum stress in endothelial dysfunction.
Cimellaro A1, Perticone M2, Fiorentino TV1, Sciacqua A1, Hribal ML3.
Author information
Abstract
AIM:
Endoplasmic reticulum (ER) stress is implicated in the pathogenesis of several human disorders, including cardiovascular disease (CVD). CVD recognizes endothelial dysfunction (ED) as its pathogenetic primum movens; interestingly a large body of evidence has identified the unchecked ER stress response as a main actor in vascular damage elicited by various cardio-metabolic risk factors. In the present Review, we summarize findings from experimental studies on the ER stress-related ED, focusing on the mechanisms underlying this association.
DATA SYNTHESIS:
Different noxious agents, such as hyperhomocysteinemia, hyperlipidemia, hyperglycemia and chronic inflammation, induce ED promoting an amplified ER stress response as demonstrated by several studies in animal models, as well as in human primary and immortalized endothelial cells. ER stress represents therefore a key mediator of vascular damage, operating in a setting of increased inflammatory burden and oxidative stress, thus contributing to foster a vicious pathogenic cycle.
CONCLUSIONS:
Experimental studies summarized in this Review strongly suggest that an unchecked ER stress response plays a central role in the pathogenesis of ED and, consequently, CVD. Counteracting ER stress may thus represent a promising, even if largely unexplored as-yet, therapeutic approach aimed to prevent vascular damage, slowing the progression from ED to cardiovascular events.
Copyright © 2016 The Italian Society of Diabetology, the Italian Society for the Study of Atherosclerosis, the Italian Society of Human Nutrition, and the Department of Clinical Medicine and Surgery, Federico II University. Published by Elsevier B.V. All rights reserved.
Definition of Endoplasmic Reticulum
Have you ever worked in or visited a large factory? If so, you probably noticed that the largest and most important area of the factory is the production space where the products are assembled. In a cell, this production space is the surface of the endoplasmic reticulum. This is where numerous chemical reactions and processes take place. Without it, production would be closed down, and the cell factory would be out of business.
Cells have many organelles that work together to help them complete their life functions. One of those organelles is the endoplasmic reticulum, which is an interconnected network of membranes used to make proteins, steroids, and lipids located near the nucleus. The surface of the endoplasmic reticulum is basically a workspace for the cell. To maximize the amount of surface area that is available the membranes are folded tightly, rather than being one flat surface.
The endoplasmic reticulum is composed of sac-like structures called cisternae that are folded and bound together. There are two types of endoplasmic reticulum: smooth endoplasmic reticulum, which has a smooth folded surface, and rough endoplasmic reticulum which has a surface studded with ribosomes, making it appear bumpy.
I can’t help but wonder if the diet also suddenly deteriorated when the USSR collapsed. It’s so hard to infer causality from correlation, though it wouldn’t surprise me in the slightest if your strain hypothesis is the main driver. I wonder if you’ve looked into diet as a possible confounder in the 1989 changes.
If you are retired and want to avoid stress, my advice is to buy a motorhome. I recommend it hugely. France, in particular, is very motorhome-friendly and the roads bear half the traffic that the English ones carry – similar population but much more space in France. (Parts of Wales and Scotland are less busy than England.) Fun, interesting and totally relaxing with plenty of opportunity to take walks, etc. and meet lots of different people. You can get information and ask advice at
http://www.motorhome-list.org.uk/
HPA stress axis leads to cellular oxidative stress. Feed your body well so that your cells can detoxify (= deal with the stress) properly.
N=1 but notable: Three of my grandparents ate white flour, real butter, ham and all the other things you can imagine and two drank Cokes daily – all three lived into their 90’s. However my other grandfather died at 44 in 1933 according to his death certificate of acute indigestion. Since he lived leading up to the depression and died during it, I assume he had the diet at the time. Depression era – No stress there – right!
My grandmother always blamed the stress of the depression on her husbands death. He had 7 kids and one on the way when he died. Their story of survival is an amazing one.
The fly in the ointment is THERE HAS ALWAYS BEEN STRESS but heart attacks are fairly modern. Some societies have been doing autopsies for thousands of years. If nothing else there is nothing in the literature about people grabbing their chest and dropping dead. There are some examples of calcium in arteries but no of fully occluded arteries. Stress of days gone by kind of pokes a hole in this unless I’m missing something?
There is a great deal about people grabbind thier chests and dropping dead. Hebreden described many cases in the Eighteenth centry. John Hunter described his angina, and died of a supposed heart attack hundreds of years ago. Autopsies on mummys from thousand of years ago demonstrate severe plaque formation.
There are just too many facts that confuse the issue. Mummies were largely from royalty and very well off. Their diet was considered vegetarian and they consumed huge amounts of sweetened breads using honey, dates and pureed fruits. It was not the commoner’s diet. They would have had much less stress at least in theory. A quote from history.com: “Examinations of mummies have indicated that many Egyptian rulers were unhealthy and overweight, and even suffered from diabetes. A notable example is the legendary Queen Hatshepsut, who lived in the 15th century B.C. While her sarcophagus depicts her as slender and athletic, historians believe she was actually obese and balding.” When looking at the bigger picture it’s impossible to rule in or out stress as it related to Egyptian Rulers but their diet was not unlike the western diet today.
There is another form of stress that’s probably to blame and that is – access for “food” 24 hours a day, 7 days a week and 365 days a year. It’s a continual feast with no famine!!! It’s the famine (or fasting) that allows our bodies to clean themselves. Not allowing our bodies to do their housekeeping has to be one of the highest forms of stress there is. Is Stress that’s created by Diet to blame – certainly a reasonable question.
-S-
“With fork and knife we dig our own graves”
These examples are in neolithic (civilized) societies. There is evidence of the truth of the poster’s assertion among paleolithic peoples (hunter-gatherers) in modern as well as past eras.
Of course, the strain theory is a good explanation of low CVD incidence in paleo peoples – stress sources were intermittent, brief and personal rather than generally traumatic over significant periods of time across the population.
Another explanation for low incidence of CVD in Paleo people is life expectancy of about 32…
Sasha, I think you need to question your assumption. There is ample evidence that both modern day paleoliths and ancient hunter gatherers were extraordinarily healthy and lived to ripe old age.
Brian, I base it on what I have read on the subject (admittedly not much). If you have links, please post them.
Sasha, I did deep dive research a decade ago so that my reading list, while long, is gone. Here’s a place to start though – http://www.beyondveg.com/nicholson-w/angel-1984/angel-1984-1a.shtml.
Thanks Brian, I read the paper but I don’t see how it refutes my point. Paleolithic adults had considerably shorter life span than modern humans. Whatever causes they died from, they simply didn’t live long enough to develop CVD at the rates that would match ours.
It makes sense to me that stress could and would play a large role in heart attacks. When I thought it over, the best counter I could think of is stress makes everything worse but isn’t necessarily a cause (just a guess of course). That mention comes from an IBD condition I have. As can be imagined those of us with stomach/GI conditions are often told our diseases can come from stress. It part it is true I say, but often I can be ill without known stresses.
Then again heart disease and IBD conditions are two entirely different conditions.
Saw the Daily Mail weighed in with their opinion on why heart disease levels have dropped.
Death rates from heart attacks and strokes plummet in a decade – thanks to medical advances and better drugs
http://www.dailymail.co.uk/health/article-3753134/Death-rates-heart-attacks-strokes-plummet-decade-thanks-medical-advances-better-drugs.html
Fantastic article again. To look at a body as a whole, emotions, everything about a dynamic complex being makes so much sense. But governments globally do not value people, this contributes to family breakdown and the repercussions on all members of the unit, children especially. Motorway driving in the UK is a nightmare, drove from Manchester to the fylde coast yesterday, dreadful, surely this is a factor for those having to journey in this country.
So enjoy all the comments from posters. thank you Dr Kendrick
Soul:
” but often I can be ill without known stresses”
Time is involved in the building and easing of diseases. (Unless, for example, someone acutely poisons you.) And the body learns to react in a certain way and needs to unlearn, sometimes needing your help. We are all conditioned by our past behaviour. Conditioning can be both useful and detrimental.
White South Africans should be a perfect test case for the stress/CVD theory (I am a white South African).
They live a typical Western lifestyle, but since majority rule in 1994 they have become politically powerless. Although their lifestyle and income levels haven’t changed much, their stress levels are much higher, being outnumbered 11 to 1 by the people they formerly oppressed.
If the theory holds, there should be a marked jump in their death rate from CVD. Any stats on this?
I think you may find it difficult to obtain stats that separate out white from black South Africans.
Re Genetics (and Larkin’s “This be the Verse”)
As stated in the blog above, the default cause when conventional risk factors don’t apply is genetics (aka an act of god or one of those things). That’s my situation anyway.
If it was genetic, why didn’t it happen at age 5, or 10 or 15? It happened at age 51. As Dr K states in “The Great Cholesterol Con”, there has to be a mechanism.
Are there any stats on cardio vascular mortality rates for under 18s? I’ll bet not many compared to age 50 and over.
And despite being told by my 2 GPS to “blame my parents” (see Larkin’s poem) and “it was one of those things”, they stuck me on statins anyway.
Hang on a second I thought, you keep telling me it was genetics that caused my cardio vascular event, why are you putting me on cholesterol lowering drugs?
Readers of Dr Kendrick and this blog will know the reason why.
Color me confused. I have no argument at all that stress is probably the biggest factor for most people. But as to diet – first of all, we now have in America an obesity and central obesity problem that is astonishing and increasing. If central obesity is associated with high cortisol, might there be other, physical (dietary) stressors that can mimic emotional stress in its effects on the body? Because not all these people are particularly stressed so far as I can tell, and it is happening at younger and younger ages. Modern life is stressful, but then that should mean that Americans heart attack rates have stayed up while Europe’s has gone down. Is that the case?
I am wondering what is going on with our health. To be sure, people are heavier and heavier, but that seems to include even people who eat sensibly. Meanwhile people like Goran and others who have lost the ability to handle carbs find that they can hardly handle carbs at all, and yet that does not seem to have been the norm in prior eras. Or was it? When you go reading around in history, the ages at death are pretty low and who knows why these people died? Some say heart attacks weren’t common in the old days, but do we even know that?
Why do we end up completely unable to handle carbs when so many cultures eat them as staples and remain thin?
I just checked my own hemoglobin a1C and it seems to be in the prediabetic range, 6.0, so now I am back to more stringent restriction on carbs. Most of my life stress has been my job. (But I’ve cut back!)
The quality of our food and the availability of fast food, frozen food and endless snacking without real family dinners and lousy breakfasts, with low fat dairy are the main culprits I think, and yet it seems to me something is missing.
I see a lot of young people who are fatter than their parents, and since this is a sign of metabolic syndrome, and metabolic syndrome is associated with diabetes and CVD, how can the rates of CVD be going down? Are people just going to die of diabetic complications instead? I am expecting the lifespan in the U.S. to plummet sometime soon. There are so many fat kids.
Anna,
Interesting thoughts, indeed!
Anna:
The Aetiology of Obesity
It has declined already. Especially for lower income whites.
And lots of what people consider “sensible eating” isn’t that at all. I treated a guy today who has the means and would be considered a sensible eater by American standards. Breakfast – cereal, bananas, coffee. Lunch – salad and sandwich. Dinner – protein (steak, etc), carb and some veggies. He’s certainly a better eater than many middle of the road Americans. Eats no fast food or processed food (except cereal), takes care of himself and has medical education to back up his lifestyle decisions. All that notwithstanding, this diet is pretty bad. Not surprisingly his digestive system is shot. Something he was surprised I picked up since he didn’t tell me about it and I didn’t ask him about his diet till I heard it in his pulse.
Which, by the way, explains many of his joint issues since these two are connected in Chinese medicine. That and being an orthopedic road kill.
He thinks he eats sensibly as probably would many others. And that probiotics do good things for him. But he does not and they do not.
Hi, are you a medical doctor.
I am not an MD, I practice Chinese medicine
any tips on reducing bp without the meds
I can’t recommend anything as far as chinese medicine without hearing your pulse. In general: read “Malignant Medical Myths” to see whether your numbers call for lowering. Don’t eat animal protein after 3pm or so, eat more soupy foods cooked from scratch. Learn to meditate – in my opinion Vipassana is best. Yoga and swimming are excellent for physical activities. If you live in a cold enough climate, participate in a “polar bear” club. Every few weeks go to a Russian or Finnish type sauna with hot/cold contrast immersions.
Studies looking at obesity discordant twins show that after a severe bout of stress the ghrelin appetite control system can be damaged and the stressed twin eats to obesity while the other twin continues to express their common genetic phenotype, namely to remain very slim.
Stress causes heart disease and stress causes obesity, so naturally therefore heart disease is statistically more common among the obese than in the slim. Obesity can indeed be described as a risk factor for heart disease (a statement which I believe has zero scientific value) but so far as I can see, no-one has successfully shown obesity is a direct cause of heart disease.
I think it’s a lot of factors. If you look at obesity, allergies, autism, and other diseases, they’ve exploded recently. When I was younger, I had no idea that people could be allergic to things. No idea of peanut allergies, milk allergies, etc. Now, we have tables at schools for those children. Something we’re exposed to has caused this (it can’t be genetics, as genetics hasn’t changed in 1-2 generations). Granted some of this is because we know about these maladies more than we did before, but I can’t remember being around more than a few children with autism. Now, I know a lot of parents of children with autism and/or allergies. We vaccinate children today with many more vaccinations then we did when I was younger.
I think there are a lot of possibilities. The current dietary guidelines in America are completely wrong, in my opinion. Grains are bad, particularly modern wheat. High omega-6 oils like soybean oil and other vegetable oils are bad. Saturated fat is not bad and likely good. High carb diets for most people (though not all) are bad. Wheat and preservatives are in everything. Try to get pickles without preservatives, for instance. Or anything prepared without wheat and soybean or other garbage oils. Could it be this? It could. Could it be vaccinations? That’s possible. Could it be overuse of antibiotics, washing our food until there’s no bacterial left on it, killing all bacteria? It could. Could it be some or all of these in combination? It could.
Personally, I now eat greens that are unwashed (I eat the dirt). I avoid taking any and all antibiotics (and the same with our kids), unless I absolutely have to take them (eg, Lyme disease). I try to get my microbiome better (although I have doubts about this too). I eat a low carb, high fat diet and perform intermittent fasting. We’ve tried to transition our kids to higher fat, lower carb diets, to the extent we can. I try to buy only organic foods, only grass-fed animals. I buy locally grown produce and animals. We try to eat more fish. We try not to eat grains at all, although that can be difficult sometimes. We try to cook all our food and buy very few things that are prepared. We try to get in the sun when we can. Has it helped? I used to take allergy pills all the time. This year, I took one pill. That’s it. I have many other improvements in my health, too, including losing 50 pounds.
“Epidemic of Absence” – great book and goes into details on many of the conditions you mention.
@BobM
>Personally, I now eat greens…dirt….low carb….high fat….fasting….organic….grass fed….local grown…. fish…not grains….not prepared.
I hope after you’ve got your waistband round that exacting list you then FEEL in control of your diet because if you don’t you’re in danger of stress-related heart disease!
Simplify life, eat what you want – with friends and a glass of wine!
Actually, the reason I started down this path is because of stress-related heart disease (idiopathic dilated cardiomyopathy). I’m now 1,000 times better than I was. And you really can’t “eat what you want”, or at least I can’t. I can’t eat high carb foods, as they cause my blood sugar to shoot through the roof, cause cravings and cause me to overeat…for days (even if I switch back to low carb). I can’t eat wheat, as I immediately get chest congestion and allergies. I can’t eat most fruits, as they cause my blood sugar to go through the roof.
You may be able to do those things, but I cannot.
I’m a scientist at heart, and attacking my issues scientifically is what makes me happy. If that doesn’t make you happy, then more power to you.
I guess an apology is due. I tried to high-jack your comment to make a point and you rightly put me in my place.
Instead reflect on a fairly recent scenario. Jamie Oliver introduces “healthy” food to a school consisting of broccoli patties with a rocket salad. The children find the food repulsive and the parents resort to passing cornish pasties through the railings to their children (I remember it happening). Once you recognise that health comes from “feeling in control” (the antithesis of stress) then you perhaps can see how much harm the health-food nazis can unwittingly do by robbing people of the food they prefer. Instead of forcing specific “healthy” food types into the nation’s diet we should be teaching children how to cook and produce for themselves the dishes that THEY find appetising.
Anna, I think that insulin resistance develops in some people sooner than in others when both have been eating a high (insulin spiking) carb diet. The cause is probably genetic. However, those cultures which thrive on a high carb diet are probably not overeating the carbs, i.e. their caloric intake is modest. It seems that insulin resistance develops after years of forcing our bodies to respond to high levels of glucose in our blood. We may have not evolved to handle this. Perhaps the carb eating cultures do not have such high glucose levels in their circulation for as long a time as some of us in North America and Europe. This is just conjecture as I have not seen any research to confirm my hypotheses, but I think it makes sense.
There ya go http://www.thefatemperor.com/blog/2015/5/10/lchf-the-genius-of-dr-joseph-r-kraft-exposing-the-true-extent-of-diabetes
PLoS One. 2016 Aug 22;11(8):e0161368. doi: 10.1371/journal.pone.0161368.
The Effect of Serum 25-Hydroxyvitamin D on Elevated Homocysteine Concentrations in Participants of a Preventive Health Program.
Pham TM1, Ekwaru JP1, Mastroeni SS1, Mastroeni MF1, Loehr SA1, Veugelers PJ1.
Author information
Abstract
Both lower serum 25-hydroxyvitamin D [25(OH)D] and elevated homocysteine concentrations are potential risk factors for cardiovascular disease (CVD). A recent analysis of the National Health and Nutrition Examination Survey reported an inverse association of serum 25(OH)D with homocysteine, however, the longitudinal relationship has yet to be investigated. We hypothesized and examined whether a temporal increase in 25(OH)D concentrations is paralleled by a reduction in the risk for elevated homocysteine. We analyzed data of 4475 participants with repeated assessments of serum 25(OH)D and homocysteine concentrations who enrolled in a preventive health program that encourages vitamin D supplementation and monitors serum 25(OH)D and homocysteine concentrations. We defined elevated homocysteine as concentrations greater than 13 micromoles per liter. Logistic regression was applied to assess the association of temporal changes in serum 25(OH)D with the risk of elevated homocysteine. We observed an inverse gradient whereby greater increases in 25(OH)D concentrations were associated with a lower prevalence of elevated homocysteine. Relative to those without temporal increases in 25(OH)D, participants who showed improvements in their serum 25(OH)D concentrations of “<25", "25-50", "50-75", and "≥75" nanomoles per liter at follow up were 0.92 (95% confidence interval: 0.62-1.37), 0.52 (0.33-0.80), 0.34 (0.20-0.58), and 0.32 (0.19-0.54) times as likely to have elevated homocysteine, respectively. These observations suggest that temporal improvements in vitamin D status reduce serum homocysteine concentrations, and therefore may potentially contribute to the primary prevention of CVD.
PMID: 27548258 DOI: 10.1371/journal.pone.0161368
Hoo ha! This is encouraging news:
http://well.blogs.nytimes.com/2016/08/23/an-unconventional-cardiologist-promotes-a-high-fat-diet/?hpw&rref=health&action=click&pgtype=Homepage&module=well-region®ion=bottom-well&WT.nav=bottom-well&_r=0
Ugh! Not so encouraging:
http://www.vox.com/2016/8/22/12552592/italy-obesity-rate
For those more interested in actual numbers than media undefined percentages the following may be of interest:
https://www.bhf.org.uk/research/heart-statistics/heart-statistics-publications/cardiovascular-disease-statistics-2015
Data can be downloaded as *xls spreadsheets.
This all adds up and I wonder if stress/ strain is cumulative Dr Kendrick? Is it likely that calcification of the arterial system builds up over many years of stress until some particular incident or period of stress tips the body over into producing a thrombus which floats off to cause a stroke or heart attack?
Another great post & one I think should be taken very seriously.
I think I am walking proof of strain & dysfunction of the HPA-axis. I could write a long essay about the strains of the last 16 years, which have been considerable & prolonged but I’ll spare you all. However, in that time, I have gone from a very healthy 30 year old to a hypothyroid 47 year old. I did a 24 hour saliva cortisol test (obviously not via the NHS, who think such things are for silly people) and my cortisol was low, low, low, low. I had a TSH of 4.9 and FT3 & FT4 were both low, but did scrape into the ranges & I do not have autoimmune thyroiditis / Hashimoto’s. Ferritin, B12, Vit D & folate all low, some below range. Sadly, my GP said I was fine & should do more exercise (walking 2-3 miles a day wasn’t good enough, I needed to do more aerobic exercise) & get more sunshine (not between 10am & 3pm though when I have my lunch hour) & everything would be fine! However, my intense irritation with the hopeless NICE guidelines for thyroid conditions is another story. So, I took matters into my own hands. I self-medicate for hypothyroidism, carefully monitoring with blood tests I pay for myself. I am also actively trying to ease the strain in my life, easier said than done, of course. I am doing my best though to go with what I can’t control & to find time to rest & not endlessly rush around, worrying about everything that hasn’t been done. (Single mum, working full-time with two children, one of whom is autistic.) I do my best to eat in a paleo style way. Lowish carb, no wheat & home cooking but I don’t put strain on myself about it. If I go to someone’s house & the food isn’t ideal, I go with it & enjoy it.
So, I see strain as hugely impactful on health. It’s already damaged mine but I’m hoping that I can take measures to alleviate that strain a bit and I won’t keel over early with heart disease.
Take long lunches, enjoy the moment, eat as well as you can & be kind to yourself!
Interesting that your GP said to stay out of the sun between 10 and 3 – the only time that the sun is over the Azimuth; the time when UVB rays hit the earth. No UVB rays; no synthesis of vitamin D.
My GP told me that there is too high a risk of burning between 11am & 3pm (I was mistaken regarding 10am, it is 11am). When I said my lunch hour was somewhere between noon & 2pm, I was told that the NICE guidelines for safe sun exposure suggest that this is not a good time to expose my skin to the sun between March & October!
Would that be the same NICE that recommends plenty of carbs for diabetics? I tend to see what NICE recommends and then do the opposite – such a rebel in my old age. Regarding sun exposure I find 10 minutes on each side like a nicely cooked sausage keeps my psoriasis more or less at bay and almost certainly boosts my vit d production, but midday it really needs to be. And, shock horror, starkers.
Nigella – I’m afraid that your GP has the wrong end of the stick! UVA rays penetrate through glass, cloud and pollution at any time, whereas UVB rays will only penetrate the atmosphere over 50º, and cannot penetrate through cloud, pollution or glass. A good rule of thumb is if your shadow is shorter than you, you will be getting UVB rays. https://www.sunsaferx.com/health-tips/vitamin-d-and-sunlight-how-to-know-if-your-sun-exposure-is-producing-vitamin-d/
Frederica, I thought it was such ridiculous advice, that I did actually check & sure enough the NICE guidelines do say that you are at risk of burning between 11am & 3pm and advise the application of sunscreen, wearing clothes & staying in the shade during those times. So it is not just my GP who will have the wrong end of the stick. (Replying to your post below, but unable to actually replay to that for some reason, hence posting it here.)
Nigella:
“I self-medicate for hypothyroidism”
How do you do that?
[Journal of the American College of Cardiology]
Volume 22, Issue 2, August 1993 >
Clinical Study | August 1993
Manifestations of coronary atherosclerosis in young trauma victims—An autopsy study
Abraham Joseph, MD, FACC; Douglas Ackerman, MD; J.David Talley, MD, FACC; John Johnstone, MD, FACC; Joel Kupersmith, MD, FACC
[+] Author Information
J Am Coll Cardiol. 1993;22(2):459-467. doi:10.1016/0735-1097(93)90050-B
Objectives. The aim of this study was to look at the prevalence of coronary atherosclerosis, its severity and site of involvement in patients 50% narrowing in 20.7% and >75% narrowing in 9%. No demographic or anatomic features seperated the groups with less or more severe involvement of their coronary arteries. Proximal involvement was more common except in the right coronary artery, which was as frequently involved distally
.Conclusions.
The overall prevalence of coronary atherosclerosis in a young, predominantly study group was comparable with that noted after the Korean War. Left main or significant two- and three-vessel involvement was noted in 20% of the group studied and emphasizes the need for aggressive risk factor modification in this group.
Good find. I think this is very interesting. The Autopsies in young men involved in the Korean war had a great impact on thinking about CVD (mainly in the wrong direction, of course).
Malcolm,
On my previous comment above you replied:
“I think that there is a difference between diet induced insulin resistnace and stressor induced insulin resistance”.
But this puzzles me since, I believe, it wouldn’t comply with Occam’s razor. And it doesn’t fit with what you have taught us -“there is a process, not a cause”. So if there is a difference between diet induced and stressor induced insulin resistance, then it looks to me as we have two different CVD diseases -which you have been arguing against in previous posts. What did I miss here? Please, comment on the difference between diet induced and stressor induced insulin resistance, so we all understand your view on this. We are all eager to learn.
Those who overproduce insulin e.g. the Pima Indians develop obesity, then insulin resistance. They have a different pathway, a different metabolic abnomrality. We call what they have, and the metabolic syndrome the same thing – but they are not the same thing. There is a whole nomenclature issue here. We call a high blood sugar level type II diabetes, and type II diabetes is a high blood sugar levels. It can have many causes, it is not always the same thing. Insulin resistance (a term I do not like) can also have many different causes, yet all causes are lumped together and called the metabolic syndrome. Some are, some are not.
What about the term “hyperinsulinemia” which Dr. Kraft seems to favour as a far better name for “diabetes type 2”?
I wonder if the earliest evidence of diabetes, the thickening of the basal lamina below the epithelium in our finest artery capillaries, which was recognised by electron microscopy carried out more than 40 years ago, is due to high insulin levels rather than the high blood sugar levels.
I have long thought this to be true. Insulin is a very powerful hormone, which also increases the risk of various cancers. It is a growth factor in many cases. I like insulin at the appropriate physiological levels, I do not like it at high levels.
Would diet induced insulin resistance do different things to your heart than stressor induced? If so, what would be different?
many things. Stessor induced would cause greater increase in clotting factors, for starters. Also more likely to increase BP and suchlike.
What accounts for this difference? Isn’t insulin insulin regardless?
There are more hormones in they body than you and I dream of Horatio.
Thank you for your reply regarding the difference between diet induced and stressor induced insulin resistance. The effect on clotting factors and BP fits beautifully into your main theme about the “process”. But I still can’t see how the metabolic problems fit into this story. Is the effect on clotting factors and BP mediated through the metabolism? Otherwise I can’t make sense of your closing statement “negative stressors can create measurable dysfunction of the HPA-axis which leads, in turn, to the metabolic problems that cause CHD”. Sorry to bother you with lots of questions, but you have awaken our quest for knowledge.
If one has OK blood pressure but DVT, is that stress related? Doer it necessarily mean clotting factor/s are high?
Hi Nigella P
Read your comments with interest, especially the hassles with 24 hour cortisol testing and blood tests (both self funded).
Having grown weary at battling for some of these tests, I, too, am looking at self funding for 24 hours cortisol (the cheapest I’ve seen online is about £90) and non standard blood tests.
Who did you choose for cortisol testing and how do you go about getting blood tests done avoiding your GP?
Personally, I think some of these tests should be automatic for those who have had cardio vascular events. I’d like my blood tests to include hs-crp, some sort of cortisol and also lp(a). Especially in the context of the polypharmacy policy when you are released. I note that Gary Taubes’ blood work results he posted on his website included hs-crp and also lp(a). Not sure if he chose a good lab or requested these though.
Thanks.
I’m not sure if I can say on here where I get my tests done. The lab for cortisol testing sounded a bit like a very famous lake in Switzerland. I had a 24 hour saliva test done. I use a different lab for blood tests. Maybe Dr Kendrick could advise on whether we are allowed to mention specific companies on his blog?
You can say. I do not allow people/companies to advertise their own products or services, but I do allow people to recommend other people’s products and services if they think they are good. It would be nuts to deny people access people to helpful things.
Too bad you aren’t in the US. There are plenty of places that will provide a doctor’s signed order so you can have tests done:
http://www.healthtestingcenters.com/
https://www.accesalabs.com/
I pay for tests myself. My GP thinks we “test too much” and wouldn’t allow me to have a hemoglobin A1C test done (but wanted to put me on statins…with low LDL, TC). My ApoB and Lp (a) are always “high” (and what’s “high” depends on the testing center), and my CRP is low-average (1.29 mg/L).
The other issue is, do any of these matter? It’s hard to know. No matter what the test, you can find a study indicating it doesn’t act as a good predictor.
Thank you Dr Kendrick for the clarification. I had my saliva cortisol tests done via Genova Diagnostics. It is possible that you may need a practitioner to use their tests. However, Regenerus Laboratories also do saliva cortisol testing & I’m fairly sure you don’t need a practitioner to use them. For my thyroid blood tests, I use Blue Horizon. You don’t need a blood draw, you can just stab yourself with a finger stabber thing that they give you and fill a small vial to send back through the post and they email you your results. I think it is a fantastic way of doing it.
Sorry–left a few paragraphs out—-Errett
Objectives. The aim of this study was to look at the prevalence of coronary atherosclerosis, its severity aid site of involvement in patients 50% narrowing in 20.7% and >75% narrowing in 9%. No demographic or anatomic features seperated the groups with less or more severe involvement of their coronary arteries. Proximal involvement was more common except in the right coronary artery, which was as frequently involved distally.Conclusions. The overall prevalence of coronary atherosclerosis in a young, predominantly study group was comparable with that noted after the Korean War. Left main or significant two- and three-vessel involvement was noted in 20% of the group studied and emphasizes the need for aggressive risk factor modification in this group.
Charles,
I am interested that you note hs-crp as something to test for. My hospital, as standard gives me readings down to 0.23 as standard. What can be more sensitive than that? Is this another scam by the owner of the test?
Sorry if this is a bit of uninformed waffle on my part but…
We’ve been alerted to studies that show that “overweight” and even obese people tend to live longer than underweight individuals. I’ve been wondering about the levels of the fat soluble vitamins (A, D, E and K) which are stored in the various degrees and types of fatness – subcutaneous v. visceral.
One might think that more fat means more vitamins?
Well this may be of interest:
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2855266/ :
“In conclusion, we found high adipose tissue concentrations of K1 and, combined with functional measures of vitamin K status, individuals with higher adiposity appear to be at risk for vitamin K insufficiency. Together, these observations may provide important insight into recent observations suggesting novel roles for vitamin K in obesity-related health outcomes (27,29). The potential inter-relationships among vitamin K, adiposity, and weight-related chronic disease merits investigation, utilizing studies that are designed to elucidate underlying mechanisms.”
Then Vitamin D3:
https://nutritionandmetabolism.biomedcentral.com/articles/10.1186/s12986-015-0019-0 :
“abdominal visceral or subcutaneous adipose tissue are inversely associated with serum 25OHD concentrations in the general adult population.”
???
Put more simply for anyone interested:
“Overweight people need fat-soluble vitamins… multiple studies have found that people with higher body-fat levels require more fat-soluble vitamins to maintain healthy blood levels of those vitamins.
Question: What are the fat-soluble vitamins?
Answer: Vitamins A, D, E and K are fat-soluble. This means that these vitamins dissolve in oils and fats, unlike the B vitamins and vitamin C, which are water-soluble. Since these four fat-soluble vitamins dissolve in fat, they are absorbed better when they are consumed with fats and oils. Once they are in the body, the fat-soluble vitamins become stored along with fat in fat cells.
Q: How does extra body fat affect the need for fat-soluble vitamins?
A: In general, it appears that someone with more body fat needs more of the fat-soluble vitamins. For example, low blood levels of vitamin D are more common in obese individuals. This may be because vitamin D gets trapped in the fat cells and is not readily available to meet the body’s needs. Consequently, obese individuals appear to require more vitamin D than someone with less body fat. This is likely the case for all of the fat-soluble vitamins, but at this time there is not enough science to know what vitamin amounts are needed by people with high levels of body fat.”
http://www.nutritionatc.hawaii.edu/HO/2010/449.htm (a resource for sports and fitness professionals – no references given)
P.S. Regarding vitamin D: obesity might therefore exacerbate the deficiency problem for dark skinned people living in sun-lacking areas?
“Health in times of uncertainty in the eastern Mediterranean region, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013”
Some snips:
“The leading cause of death in the region in 2013 was ischaemic heart disease (90·3 deaths per 100 000 people), which increased by 17·2% since 1990”.
“The leading cause of disability-adjusted life-years (DALYs) was ischaemic heart disease for males and lower respiratory infection for females. High blood pressure was the leading risk factor for DALYs in 2013, with an increase of 83·3% since 1990”
http://www.thelancet.com/journals/langlo/article/PIIS2214-109X(16)30168-1/abstract
F.A.O. Mr Chris and hs-CRP blood test
My understanding is that there are 2 types of c reactive protein (CRP) blood tests:
1. standard CRP and
2. high sensitivity CRP
These are inflammation tests but the hs-crp is used to test for risk of heart disease. The ranges are as follows (quoting from Gary Taubes’ results from Quest Diagnostics):
a. 3.0 to 10.0 mg/l = higher relative cardiovascular risk.
Taubes’ result was 0.72 mg/l and yours was 0.23 mg/l – both less than one.
Lab tests online website has a detailed q&a on this and worth a general google anyway. I think Dr Kendrick has blogged/written/commented upon inflammation and (possibly) crp testing too.
I collapsed unexpectedly at work in April with no warning and no conventional risk factors. Very worrying! So, for my own peace of mind, I’m trying to get these sort of tests done. Comments posted in Dr Kendrick’s previous blog on diet mentioned the lp(a) hypothesis of CVD which I wasn’t aware (vitamin c deficiency plays a role) and this can be tested for.
Hope this helps.
Charles
I assume there is only one protein. If my blood test measues down to 0,23, that seems pretty sensitive to me, so why do I need something else?
Heart. 2016 Aug 22. pii: heartjnl-2016-309573. doi: 10.1136/heartjnl-2016-309573. [Epub ahead of print]
Trends in the epidemiology of cardiovascular disease in the UK.
Bhatnagar P1, Wickramasinghe K1, Wilkins E1, Townsend N1.
Author information
Abstract
Cardiovascular disease (CVD) mortality in the UK is declining; however, CVD burden comes not only from deaths, but also from those living with the disease. This review uses national datasets with multiple years of data to present secular trends in mortality, morbidity, and treatment for all CVD and specific subtypes within the UK. We produced all-ages and premature age-standardised mortality rates by gender, standardised to the 2013 European Standard Population, using data from the national statistics agencies of the UK. We obtained data on hospital admissions from the National Health Service records, using the main diagnosis. Prevalence data come from the Quality and Outcome Framework and national surveys. Total CVD mortality declined by 68% between 1980 and 2013 in the UK. Similar decreases were seen for coronary heart disease and stroke. Coronary heart disease prevalence has remained constant at around 3% in England and 4% in Scotland, Wales, and Northern Ireland. Hospital admissions for all CVD increased by over 46 000 between 2010/2011 and 2013/2014, with more than 36 500 of these increased admissions for men. Hospital admission trends vary by country and CVD condition. CVD prescriptions and operations have increased over the last decade. CVD mortality has declined notably for both men and women while hospital admissions have increased. CVD prevalence shows little evidence of change. This review highlights that improvements in the burden of CVD have not occurred equally between the four constituent countries of the UK, or between men and women.
Published by the BMJ Publishing Group Limited. For permission to use (where not already granted under a licence) please go to http://www.bmj.com/company/products-services/rights-and-licensing/
KEYWORDS:
Stroke
Personally I prefer the actual numbers. Once one gets into “standardized” rates one has to know precisely what and how the data has been manipulated, A classic example is the us of relative rates, ORs, and HRs. A useful example is given by Gigerenzer in his book “Risk Savvy…” where the contraceptive pill was reputed to increase breast cancer by 100%. The actual numbers were an increase from 1 per 7000 to 2 per 7000, a 100% RELATIVE increase. Consequences were a substantial rise in abortions and unwanted babies.
From the BHF morbidity spreadsheet the increase in the UK rose from 920216 in 2010/2011 to 956757 in 2013/2014 a rise of about 1% per year for 4 years. Now of course that can be manipulated in various ways such calling 1% “more or less” stable or adjusted by population age etc. The raw mortality spreadsheet also shows the massive decrease that has occurred but surely that is due to improved therapy, not prevention with increasing metabolic syndrome, insulin resistance, obesity and diabetes all of which contribute to the morbidity of CVD?
Sasha,
Please explain more about how you practice Chinese medicine and how you learn it.
What do you listen for in the pulse and what about feeling the pulse as the Indians do?
Why would probiotics not do a body good?
You are saying that the digestion system and joints are connected?
Anna, it would be hard to explain online what I listen for in the pulse since pulse diagnosis is best learned hands on.
People qualify to practice Chinese medicine after a 3 or 4 year program in a school (in China or most major European and North American countries). Lots of that time spent in school is kind of a waste but that’s probably true of many other types of schools. Overall, mastering Chinese medicine is a life long learning which is kind of cool, IMO.
I am not familiar with Ayurvedic pulse diagnosis but I do know there are differences with TCM diagnosis.
I don’t believe in probiotics because I believe that things made by nature are superior to things made in a lab. I recommend fermented foods, soupy foods, kefir, yogurt, etc. And eating according to a particular regimen which will help the body grow healthy microbiome.
In my experience joint issues and digestive system issues often present together. I recently had a patient with chronic pain in the joints of the feet. He also had week Spleen/Stomach pulse. He was advised to have surgery on his feet (it’s fee for service system in the US so it’s crazy the recommendations people get). All he needed was a few acupuncture treatments and dietary recommendations that take into account where he lives and his body constitution.
Dr Kendrick, first thank you for your work and communicating it to us all! I wonder if you could check out and comment on the following study I saw referenced in the New Scientist recently, embedded in an article claiming that after all replacing saturated fats with poly or mono unsaturated fats reduced the incidence of CHD
http://archinte.jamanetwork.com/article.aspx?articleid=2530902
I am a biological scientist and have been horrified to discover down the years what constitutes research and claims based on this research down the years. I first became aware of this when I was diagnosed with hypothyroidism in 1985, responded erratically to levo thyroxine replacement therapy but was stone-walled by ALL specialists when I attempted to reason over my response and ask fundamental questions about their claims and the basis of their claims – a long story and not relevant here, but discovering your reasoning re CHD was a further shock – why had I assumed such shoddy work and blind faith in established models was confined to endocrinology!!!?????
I follow your quest with great interest and try to share it with others…
I will have a look at it.
Sue M,
Have a look at this link and comments. They reflect my own sentiments about this paper. https://pubpeer.com/publications/AF5BEE6A918463C67C2758AE4E47CD
Dr. Kendrick,
Perhaps a good topic for an upcoming post might be about diet induced insulin resistance versus stress induced, and also why you don’t like that term.
It gets complicated. My main problem is that it places insulin at the heart of every discussion. Insulin is but one player. Glucagon, for example, is more important. It is much more important to keep blood sugar levels up, than to reduce them. Ten minutes of severe hypoglycaemaia, and you will be severely brain damaged, or dead. You can live with twenty years of raised blood sugar levels. Which is probably why nature only gave us on main blood sugar reducing hormone, and four that keep blood sugar levels up. The human brain is a harsh metabolic master.
Dr Kendrick
As usual you have produced another stimulating article for which I am truly grateful. I look forward to the book in due course.
However I would be interested to know more about glucagon and leptin and their involvement in general health and CVD and Alzheimer’s in particular.
One further question: Can either glucagon or leptin be measured and if so are either provided by the NHS as standard tests or is their importance simply ignored?
They can be measured, but they are ignored by the NHS at present.
Where does gherlin fit in? As the ‘hunger hormone”, is it one of the hormones keeping blood sugar levels up?
Med Hypotheses. 2016 Jul;92:7-11. doi: 10.1016/j.mehy.2016.04.033. Epub 2016 Apr 20.
Dairy products and the French paradox: Could alkaline phosphatases play a role?
Lallès JP1.
Abstract
The French paradox – high saturated fat consumption but low incidence of cardiovascular disease (CVD) and mortality – is still unresolved and continues to be a matter of debate and controversy. Recently, it was hypothesised that the high consumption of dairy products, and especially cheese by the French population might contribute to the explanation of the French paradox, in addition to the “(red) wine” hypothesis. Most notably this would involve milk bioactive peptides and biomolecules from cheese moulds. Here, we support the “dairy products” hypothesis further by proposing the “alkaline phosphatase” hypothesis. First, intestinal alkaline phosphatase (IAP), a potent endogenous anti-inflammatory enzyme, is directly stimulated by various components of milk (e.g. casein, calcium, lactose and even fat). This enzyme dephosphorylates and thus detoxifies pro-inflammatory microbial components like lipopolysaccharide, making them unable to trigger inflammatory responses and generate chronic low-grade inflammation leading to insulin resistance, glucose intolerance, type-2 diabetes, metabolic syndrome and obesity, known risk factors for CVD. Various vitamins present in high amounts in dairy products (e.g. vitamins A and D; methyl-donors: folate and vitamin B12), and also fermentation products such as butyrate and propionate found e.g. in cheese, all stimulate intestinal alkaline phosphatase. Second, moulded cheeses like Roquefort contain fungi producing an alkaline phosphatase. Third, milk itself contains a tissue nonspecific isoform of alkaline phosphatase that may function as IAP. Milk alkaline phosphatase is present in raw milk and dairy products increasingly consumed in France. It is deactivated by pasteurization but it can partially reactivate after thermal treatment. Experimental consolidation of the “alkaline phosphatase” hypothesis will require further work including: systematic alkaline phosphatase activity measurements in dairy products, live dairy ferments and intestine of model animals. Furthermore, stool residual IAP, a possible early marker of diabetes, should be assayed in human cohorts. If confirmed, this “alkaline phosphatase” hypothesis will highlight the protective effects of milk alkaline phosphatase and promote the consumption of (microbiologically safe) raw milk and dairy products. Microorganisms secreting alkaline phosphatases may be privileged as ferments in dairy products.
Copyright © 2016 Elsevier Ltd. All rights reserved.
KEYWORDS:
Alkaline phosphatase; Cheese; Dairy products; French paradox; Milk
There is only a French paradox, and any need to explain it, if you believe that saturated fat caused CVD.
Very true—I’m in the hyper-lipid camp myself—-macros 70%SF—20%P—10%chocolate + some veggies & a beer or two 🙂 I enjoy your essays very much—-continue the good fight—Clan McBean in the USA
Errett,
As usual an interesting contribution but as it is behind a paywall the full benefit remains unknown
As Dr Kendrick in his book “The Great Cholesterol Con” pointed out many other countries with high saturated fat intake have the same results. The report was the WHO-BHF Monica study which was published two or three times as updates. I used multiple regression on the data for carbs, total fat and fruit&veg proportions of some 40 countries versus their CVD levels. The result showed that carbs were positively associated with CVD while Total Fat and Fuit&veg were negatively associated. Saturated Fat in the early reports was also negatively associated with national levels of CVD but this factor was leftt out in later updates. More agnotology.
Wait a minute here, people in France, Spain & Italy to name a few, eat a lot of Carbs, Bread, Pasta, Croissants, pastries and so on. But people in France still have the lowest rates of CVD.
Scientists have long known that infants born to women who are obese show higher risks of obesity, but they don’t fully understand what boosts those risks. Researchers at Joslin Diabetes Center now have demonstrated that umbilical cells from children of obese or overweight mothers show impaired expression of key genes regulating cell energy and metabolism, compared to similar cells from babies of non-obese mothers.
Such findings may help to pave the way toward improved healthcare, both before and after birth, for children at heightened risk of obesity, says Elvira Isganaitis, M.D., M.P.H., Assistant Investigator and Staff Pediatric Endocrinologist at Joslin Diabetes Center and Instructor in Pediatrics at Harvard Medical School, and corresponding author on a paper about the work published in the International Journal of Obesity.
The Joslin study also suggests that the increased risks of obesity may be driven by boosted levels of certain lipids (fats and other substances that are not soluble in water) in the maternal blood that flows through the umbilical cord, says Isganaitis. A research associate and staff endocrinologist at Joslin, she is an instructor in pediatrics at Harvard Medical School.
Suzana Maria Ramos Costa, M.D., Ph.D., of Joslin and the Federal University of Pernambuco in Recife, Brazil, who is co-first author on the paper, began the research by gathering umbilical cords after birth from healthy Brazilian women without diabetes. Costa recruited 24 overweight or obese women (with a body mass index over 25 before pregnancy) and 13 women who were not overweight for the study.
The scientists collected umbilical cells from the vein that carries oxygen and other nutrients from the placenta to the embryo. “These samples give a window into the nutrients and metabolites that are coming from the mom into the infant,” says Isganaitis.
The Joslin team discovered that in these cells, increased obesity in the mothers correlated with lower expression of genes regulating mitochondria (which act as the cell’s powerhouses) and of other genes regulating the production and metabolism of lipids.
“This suggests that already at birth there are detectable metabolic perturbations resulting from maternal obesity,” she says. Changes in these cells were similar to some known to occur in obesity, insulin resistance and type 2 diabetes, she adds.
When the researchers followed up by analyzing fetal blood from the umbilical cord vein, “we found that the infants of obese mothers had significantly higher levels of many lipids that are known to be metabolically deleterious, like saturated fatty acids,” Isganaitis says. Fat tissues in the obese mothers may shed fatty acids that make their way into the fetal blood and create a kind of “fuel overload” for the embryo, she remarks.
Isganaitis and her colleagues will carry out further research on umbilical cells and blood among Boston newborns to see if the study results are confirmed in this population. She also plans similar analyses for children born to mothers who have either gestational diabetes or type 1 diabetes.
Additionally, Isganaitis is examining how such prenatal exposures may encourage certain stem cells found in umbilical cords, which can differentiate into various types of tissues, to preferentially turn into fat cells.
She hopes that eventually it will be possible to use blood markers to identify embryos at risk for obesity or related conditions such as type 2 diabetes, and to follow up with suitable medical interventions.
“Pregnant women engage often with their healthcare providers, and you can really tap into their motivation,” she says. “If we could come up with tailored interventions — if we could say, take this vitamin, exercise regularly and you can minimize obesity or diabetes risk in your child — I’m sure mothers would do it.”
Isganaitis adds that mothers and healthcare providers also could carefully monitor the growth patterns and nutrition of children at risk of obesity, both in the first two years of life and afterwards. “Your risk of chronic diseases isn’t set in stone at birth; there are many different periods in which your lifelong disease risk can be modulated,” she emphasizes.
Story Source:
The above post is reprinted from materials provided by Joslin Diabetes Center. Note: Content may be edited for style and length.
There is definitely a connection between inflammation and psychological stress – Anxiety/depression etc. I’ve written a bit about it in other places
But the problem is which is the cause and which is the effect. Even the antidepressant drugs – which often reduce inflammation – is that how they actually work? Or is it a secondary effect? So the new work on ketamine – treats depression rapidly – but medicine has known that ketamine is a strange anesthetic – as it reduces inflammation – sometimes used for that effect in surgery.
If one thinks about the definition of depression – it is the same as an immune response, but lacking the fever and WBC. People that undergo interferon therapy suffer depression. So is depression really a disease of the immune system? Again – the arrows of causation are not clear. We can create many narratives – but there needs to be quality, sane, and non politicized research to untangle these threads.
A couple of other bits – fish-oil is thought to prevent/treat depression – also reduce some inflammation – which might be the cause and which the effect?
I wonder about “believing”!
I fully agree with Malcolm (and actually the “health care system” in this specific case) that stress is a long and a short time “killer” and this agreement is not least based on my personal experience which I think creates strong (religious?) beliefs.
Where we may be in disagreement is about the important role of diets on the health status where I myself sides with Hippocrates both in the “prophylactic” way and as a remedy and on this subject my belief is again strongly reinforced by the “chocking” improvements experienced by me and my wife.
So – I have turned fundamentally interested in the subject of the effect of nutrition on health. Since my tooth health has finally been completely restored after 40 years of constant struggle as a part of the “chock” and where the strict LCHF-culture seems to have done it.
I have now written a new chronicle on this happy tooth outcome event at Dr. Annika Dahlqvist’s blog which I value as high as Malcolm’s blog.
For those who may be interested and don’t happen to master our beautiful Swedish language may try the Google translation feature for what it is worth by pressing the button to the right “ÖVERSÄTT” and get an idea what it is all about.
Most of my chronicle is based on the experience of the acknowledged “bets dentist in the world” a hundred years ago who wrote a famous classic book after having visited the remains of many “natural peoples” around the world to find out the impact of modernised food on the health status. The scientific dentist was Weston Price and the book “Nutrition and Physical Degeneration” – ” A comparison of Primitive and Modern Diets and Their Effects” and those of you who are familiar with the most famous french physiologist Claude Bernard may also appreciate the same scientific rigour reflected in Price book.
I think the quality of the carbohydrates we eat matters a lot too, its not just the carbohydrates themselves. I think eating 3 bananas a day will never have adverse ill effect while eating 3 candy bars will, especially tooth decay. No?
A carbohydrate is a carbohydrate. The digestive system takes them all (apart from very tightly bound complex-carbs, which cannot be digested) and breaks them down into glucose and/or fructose.
I suspect that it would be less BG disruptive to eat the banana skin rather than the banana – a shame really; I do miss banana and honey sandwiches (the bad old days.) Gee whizz, I’m so virtuous these days.
Maybe from a strict biochemistry point of view. But i don’t think bananas will cause tooth decay, or ill side effects, while sodas and candy bars will. Why? for many reasons. What we find in fruits, the fibers, the enzymes, natural minerals, antioxydants and so on, won’t be found in sodas or refined sugars. This is what i meant by ‘quality’.
I’m about halfway through Kendricks’ ‘The Cholesterol Con’, and I now see why diet is not the immediate cause of CHD, except: by diet, do we exclude sugar and the chemicals in processed foods? Do we exclude all the chemicals in our air, water and soil? Aren’t they too, part of our ‘diet’ every time we breathe, eat and drink?
And what of stress as major cause of CHD? Difficult to measure I know, but stress does raise blood pressure and unleash a rack of quite powerful chemicals into the bloodstream. Stress interferes with sleep, digestion, even breathing…
personally i would never give up organic honey and maple syrup, just to be on a lchf diet, its ridiculous. Both are elixir of health, i cant think of something more healthy than honey. Might as well start saying that all the wonderful fruits we found across the planet are poison for human beings, i mean c’mon.
as a side note, I will take a jar of honey anytime before a steak from a soy or corn fed cow, injected with growth hormones to grow twice as fast, and injected with antibiotics non-stop till the day shes slaughtered.
A snippet –
Have just read this about shrews:
“Being extremely small, they have the highest metabolic rate of any animal and are active throughout the year – hence their lifespans are usually limited to a maximum of one year.”
Comparing this with the Greenland Shark, the oldest vertebrate we know of (400 year lifespan):
“Researchers believe that the secret behind the longevity of these sluggish fish that are often called “sleeper sharks,” is the frigid waters of the Arctic and North Atlantic where they reside. Michael Oellermann, a cold-water physiologist at Loligo Systems in Viborg, Denmark, says the temperature helps slow down their growth and biochemical activity, extending their lifespan.”
Perhaps being sluggish is not such a bad thing!
Is there evidence based data to support the regimen of beta blockers paired with blood thinners as treatment for CVD event?
From Errett
August 25, 2016 at 10:02 pm
When I read this excerpt, I took in a deep breath.
<>
This really is conjecture with little evidence to support it and the assertion that saturated fat is metabolically deleterious is likely going to lead them down the wrong path of discovery just as happened with “saturated fat is bad” in adults.
What might be far more informative would be to see how glucose/insulin pathways are modulated in umbilical vein cells (and other places). The fetus uses glucose as its main source of fuel and fat utilization is for structural purposes, not energy. We have a long way to go.
I’d like to read some detail about how our autonomic nervous systems might effect outcomes of stress. If our sympathetic systems are in high tone, ready to fight or fly in a split second, that can’t be good. “Autonomic dysfunction” shows up in the literature a lot more often than any cogent suggestion as to how to address it.
Dr Kendrick?
Anyone??
Yoga, exercise, TM, good social support, CBT, breathing exercises, getting a pet, joining a club, and suchlike.
I understand fully that you cannot diagnose or give specific advice at this remove. There is no magic pill. However, your brief list seems like a band-aid for a system that’s essentially broken.
Me, just as an example of what I mean:
I do much of what you suggest already.
I’ve given up going to the movies. I could bear up to my heart slamming in my chest when I was younger, watching Sigourney Weaver’s close calls in “Alien”. Not any more. Now I have to be careful reading an Ian Rankin novel. My heart rate soars. And skips. Just sitting there reading.
White coat syndrome of 160/100 in my Dr’s office; 118/75 at home relaxed.
TM doesn’t work out in the World. Getting a pet doesn’t come close.
Surely this describes a general organic problem explaining “strain” for which there are more direct treatments?
Live a life that reduces external stressors as much as possible – at least long term negative stressors. This is obviously very personal, and general advice can only be general advice. Some people react more, and badly. Other react more positively. There can be no absolutes here.
Dr K
Would you allow me to add to your list of advice for a long happy life?
Eat real food, in reasonable quantities, nothing too much.
And one that you cannot put:
If you are on life long medicine., find out all you can about why, side effects, and are there people who have got off life long medicine by controlling their condition in other ways.
I would agree
The yoga studio I attend is instituting a new class called Balancing the Nervous System–a combination of active and restorative poses. Maybe the word is getting out. The teacher who developed the class says a lot of his students work in the tech industry, outrageous number of hours per week, are chronically exhausted but can’t relax.
Is the apparent standard treatment of a CVD event of beta blockers and blood thinners based in any reliable research? Doesn’t make a lot of sense to slow the heart and thin the blood!
Well, it does make sense to reduce blood clotting propensity. As for slowing the heart, the benefit of beta-blockers is not slowing the heart, but altering various other parameters e.g. pre-load. There is also benefit from reducing the risk of various arhythmias.
Such intervention might help a bit – but there are many that are predisposed – genetically? or via earlier exposure to pathogens? Or some vagus nerve connection? Even if exercise lowers it a bit – it is really not enough.
There are meds that do reduce inflammatory markers – some antidepressants – some antibiotics, low dose ketamine – but we don’t have any basic data on meaningful outcomes. The NSAIDs probably work but my hunch is the later rebound is doing even more harm ( ringing a control loop) and I think their effects are transient – not something that is effective long-term.
My hunch is when we peel back the layers, we will find that much of what we call depression and anxiety disorders today are actually caused by inappropriate immune system responses – I don’t think today’s medical community is in any position to know how to treat these disorders. We must be very careful to label any narrative as speculative when it is – there are no end of narratives one can buy into – humans are susceptible to many cognitive biases – wanting to know even when knowing is not possible.
The problem is also partly the patients – they are demanding the “SOMETHING” be done – when the reality is interventions often come with potential risks that outweigh the potential benefits. Telling a patient that there isn’t anything that we know of today that will make a big difference is not an easy job – but often is the right thing to do.
Beta blockers,
It’s long been known that severe performance anxiety (Stress?) of musicians can be “managed” with a pre-event dose of propranolol. My cardiologist suggested metoprolol for my physiological over-reaction to various life situations. My prior experience with metoprolol left me physically and emotionally debilitated.
So, it’s either that medical sledge hammer or get a new life.
Try meditation
JDPatten, and Malcolm
I wonder if the stress involved in going to see a scary movie -if this is what you like (as opposed perhaps to accompanying someone else who enjoys such movies) – is actually harmful. After all, you don’t leave the cinema worrying about meeting one of those Alien creatures! Wouldn’t this count as a positive stressor?
It could well do so. We need a certain amount of stimulation. Scary movies are probably quite good for you. I await evidence of course.
Positive stressors. That’s a nice idea. What if the “positive” stressors are often and exaggerated? Not so positive?
Interesting subjekt indeed. Dr. Sroka adressed this issue profoundly and it has been brought up a couple of times here. He wrote a very interesting paper about the connection with MI some years go.
Malcolm’s suggestions are along these lines.
There are external events which Dr Kendrick calls stressors and there are internal hormones which he calls strain. To have a proper understanding of stress you need to realise that the crux of the matter is the bit in-between these two, namely how you FEEL about external events. In turn, the major determinant of how you feel about external events is how you feel about your self: your degree of self-esteem. For example someone with low self-esteem might be insulted at school and have the reaction “That was the worst thing that’s ever happened to me, now I’m afraid to go back to school in case it happens again”; that person will suffer great strain as a consequence. By contrast someone with high self-esteem might encounter the same external event (the insult) and react with the thought “I always knew that girl was foul mouthed” and as a consequence suffer no strain whatsoever. In response to the precisely the same external stressor, one person encounters a great surge of stress hormones, the other person reacts like a military tank which comes under fire from rifle bullets – ping, ping go the deflections.
Dr Kendrick has stated in this blog that the way to preserve your coronary health is to reduce external stressors. I’m sorry to say I completely disagree. The way to reduce stress is to change the way you FEEL about external events by changing your attitude to them. Grossarth-Maticek’s experiment was incredibly important because he proved scientifically that it is possible to dispel 4 out of every 5 cardiovascular events and 10 out of every 11 cancers simply by manipulating an individual’s attitude to external events.
Having recognised that low self-esteem is effectively the source of most heart attacks and of most cancers, one might conclude that the solution would be to encourage high self-esteem. My contribution to the topic is to suggest that high self-esteem (an arrogant, sense of entitlement) then becomes the source of all the suffering which the powerful elite inflict on others. High self-esteem is the platform from which employer inflicts stress on employee, businessman exploits customer, teacher abuses child and doctor fails patient. The real answer to the human conundrum is to encourage a sense of EQUAL self-esteem, to encourage the condition characterised by “Love Thy Neighbour as Thyself”. Equal self-esteem is a very contented condition which is remarkably free from stress and consequently free from CVD and cancer but the egalitarian is uniquely of great benefit to society at large. Humanity’s “Great Souls” such as Gandhi and Mandela, who proved capable of enhancing the self-esteem of whole nations, these spiritual souls are first and foremost egalitarians. For what it’s worth I suspect Dr Kendrick also has a highly developed sense of egalitarianism – the good guys always have.
I agree that your reaction to stressful events is, in fact, key. However, it is probably best to resign and avoid a bullying boss, rather than rely on your own sense of self-worth, which can be destroyed over time by really horrible people.
Very good points.
I think there need to be a difference in self-esteem and big egos. self worth and Egos are 2 things. One can have a very poor self-esteem and a huge ego (failing to learn from mistakes for example) Or one can have a good self-esteem ( confident of his abilities in general, willing to learn etc. ) but have a very little ego.
Can someone help me interpret the conclusions to be drawn from the last two posts. Dr. K seemed to downplay the role of diet in CVD in the prior post. And here he seems to be making the case for a strain based causality. Is he positing that that poor diet is can contribute to CVD because it is a strain/stressor. But that diet is just one type of strain/stressor and perhaps not the most powerful or important one?
While this comment is off topic it is another example how data can be interpreted to inflate risk, stress/strain and scare patients unnecessarily. The medical establishment is no longer interested in individual patients, only the herd.
http://www.telegraph.co.uk/science/2016/08/22/hrt-triples-the-risk-of-breast-cancer-longest-ever-study-shows/
HEADLINE
HRT triples the risk of breast cancer, biggest ever study shows
Now new findings by the Institute of Cancer Research and Breast Cancer Now suggest the original risk had actually been underestimated.
A study of 100,000 women over 40 years found those who took the combined oestrogen and progestogen pill for around five years were 2.7 times more likely to develop cancer compared to women who took nothing, or only the oestrogen pill.
The risk rose to 3.3 times for women who took the drugs for 15 years or more.
Around 14 in 1,000 women in their 50s are expected to develop breast cancer, but that rises to 34 in 1000 for women taking the combined pill, the study suggests.
Comment: 34/14 = 2.43 times or 243% greater risk
Alternatively the REAL difference is (34-14) per 1000 = 20/1000 or just 2% increased risk or just 1 in 50 at greater risk leaving 49 out of 50 (980/1000) without increased risk; i.e. a probability of 0.98 of not suffering cancer or the adverse events of the menopause.
I wonder what advice a GP would give based on the formal advice. “Three times greater chance of cancer or a 2% greater chance?”
Or an increase in life expectancy – which was the main finding
Thanks for that info, Dr Kendrick! I think I would be headed for a memory care facility without hrt. Starting it again now in my seventies snapped me right back so I would take it anyway, but now without the fear.
Mike—Very helpful—it certainly benefits all of us if we develop the skill to analyze the data from these studies—“Lies, damned lies, and statistics”—–especially since it seems most are flawed in some way.
Article Explains Importance of Heart Rate Variability for Your Health
January 26, 2015 Science of the Heart 43513
Article Explains Importance of Heart Rate Variability for Your Health
It has only been five decades since scientists began to alter their long-held belief that the human body’s cells, tissues and organs, particularly the heart, strive to maintain a constant static or steady state.
“We now know that the normal resting rhythm of the heart is highly variable rather than being monotonously regular, which was the widespread notion for many years,” write the authors of a new article slated to appear in the January issue of Global Advances in Health and Medicine (GAHM), a professional journal.
Variability in heart rhythms, which is gaining scientists’ attention around the world today, is the subject of their article, Heart Rate Variability: New Perspectives on the Physiological Mechanisms, and Assessment of Self-Regulatory Capacity and Health Risk. The authors are HeartMath Institute (HMI) Director of Research Rollin McCraty, Ph.D. and Fred Shaffer, Ph.D., BCB of the Center for Applied Psychophysiology, Truman State University, Kirksville, Mo.
Heart rate variability, the change in the time intervals between adjacent heartbeats, is directly related to the body’s interdependent regulatory systems and ultimately, their efficiency and health. “An optimal level of HRV within an organism reflects healthy function and an inherent self-regulatory capacity, adaptability, or resilience,” McCraty and Shaffer write.
Although generally the greater the HRV, the better, they note that too much variability, or instability “such as arrhythmias or nervous system chaos is detrimental to efficient physiological functioning and energy utilization… “Too little variation indicates age-related system depletion, chronic stress, pathology, or inadequate functioning in various levels of self-regulatory control systems.”
The GAHM article cites much of the pivotal heart rate variability research since 1965, when HRV began to be recognized for its importance in indicating or predicting various risk factors. Among these are fetal distress, autonomic nervous system dysfunction, heart disease, anxiety, depression and asthma among other health conditions.
Many studies, including some conducted by McCraty and others at HMI, correlate an optimal level of HRV, or HRV coherence and coherence training, such as that using HeartMath self-regulation techniques, to a variety of benefits. Among the results of these studies were enhanced cognitive function in a range of age groups and greater functional capacity in heart-congestive patients.
This link shows how coherence training in students is actually effected—-
https://www.heartmath.org/programs/education/emotion-self-regulation-technology/
Improvements were demonstrated in a study employing coherence training with a group of middle school students with attention-deficit hyperactivity disorder. Improvements were shown in their short- and long-term memory, ability to focus and behaviors at home and school.
“A study of recently returning soldiers from Iraq who were diagnosed with PTSD,” the article states, “found that relatively brief periods of HRV coherence training combined with practicing the (HeartMath) Quick Coherence® Technique resulted in significant improvements in the ability to self-regulate along with significant improvements in a wide range of cognitive functions, which correlated with increased cardiac coherence.”
A range of positive health-related outcomes also has been demonstrated in studies with correctional officers who participated in coherence training, McCraty and Shaffer explain. In one study conducted by McCraty, correctional officers improved their blood pressure, total cholesterol and fasting glucose levels and reduced overall stress and fatigue. Similar results were achieved with police officers.
In conclusion, McCraty and Shaffer write, “Numerous studies have provided evidence that coherence training consisting of intentional activation of positive emotions paired with HRV coherence feedback facilitates significant improvements in wellness and well-being indicators in a variety of populations.”
HEALTHHEART RATE VARIABILITYHRV STUDIES
I have met McCraty a few times. I think his work on HRV and trying to use various methods to improve HRV is very important
What about the connection between HRV and acute MI? Dr. Sroka “special”?
Int J Occup Med Environ Health. 2015;28(1):42-51. doi: 10.2478/s13382-014-0289-1.
Prolonged job strain reduces time-domain heart rate variability on both working and resting days among cardiovascular-susceptible nurses.
Borchini R1, Bertù L1, Ferrario MM2, Veronesi G1, Bonzini M1, Dorso M3, Cesana G3.
Author information
Abstract
INTRODUCTION:
Modifications of hearth rate variability (HRV) constitute a marker of the autonomic nervous system (ANS) deregulation, a promising pathway linking job strain (JS) and cardiovascular diseases (CVD). The study objective is to assess whether exposures to recent and prolonged JS reduce time-domain HRV parameters on working days (WD) among CVD-susceptible nurses and whether the association also persists on resting days (RD).
MATERIAL AND METHODS:
313 healthy nurses were investigated twice with one year interval to assess JS based on the demand-control and the effort-reward models. 36, 9 and 16 CVD-susceptible nurses were classified as low JS in both surveys (stable low strain – SLS), recent high JS (high JS at the second screening only-RHS) and prolonged high JS (high strain in both surveys-PHS), respectively. In 9, 7 and 10 of them, free from comorbidities/treatments interfering with HRV, two 24-h ECG recordings were performed on WD and RD. Differences in the time domain HRV metrics among JS categories were assessed using ANCOVA, adjusted for age and smoking.
RESULTS:
In the entire sample (mean age: 39 years, 83% females) the prevalence of high job strain was 38.7% in the second survey. SDNN (standard deviation of all normal RR intervals) on WD significantly declined among JS categories (p = 0.02), with geometric mean values of 169.1, 145.3 and 128.9 ms in SLS, RHS, PHS, respectively. In the PHS group, SDNN remained lower on RD as compared to the low strain subjects (142.4 vs. 171.1 ms, p = 0.02). Similar findings were found for the SDNN_Index, while SDANN (standard deviation of average RR intervals in all 5 min segments of registration) mean values reduced in the PHS group during WD only.
CONCLUSIONS:
Our findings suggest that persistent JS lowers HRV time-domain parameters, supporting the hypothesis that the ANS disorders may play an intermediate role in the relationship between work stress and CVD.
This work is available in Open Access model and licensed under a CC BY-NC 3.0 PL license.
KEYWORDS:
ECG-monitoring; HRV; Heart rate variability; job strain; nurses; time-domain parameters
PMID: 26159946 DOI: 10.2478/s13382-014-0289-1
In depth explanation of HRV and health:
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4311559/
Donald Trump is taking a statin. Should we be worried? Will he remember where he wants to build a big wall?
Stephen;
Given the paranoia over cholesterol in the states one suspects that anyone over 50 is likely to be on statins, particularly politicians, which may account for some of the mess they have got the world into.
inflammation – incident ischemic stroke. Higher levels of 4 biomarkers-CRP, tHcy, TNFR2, and VEGF-increased risk of IIS and improved the predictive ability of the Framingham Stroke Risk Profile score. http://www.ncbi.nlm.nih.gov/pubmed/27558379
good info—helpful Thanks
Bovril, mince pie. What about haggis?
Haggis is good for you… like Guinness.
If it’s cortisol could we see higher rates of CVD amongst those with depression particulary if it’s chronic? Clearly medication may cloud everything.
We do. In fact, depression can actually cause people to have a high enough blood sugar level to be diagnosed as having type II diabetes.
How do we know that?
For JDPatten re: “My heart rate soars. And skips. Just sitting there reading.”
If you don’t mind my giving you my two pennies worth: Do try to not see this heart behaviour as a defect which threatens your life but rather as your body’s conditioned reaction to excitement – which of course, it is. We build up our reactions over time. Try not to be anxious about these short-term reactions. We all have them to varying degrees. Take some unaccustomed action. Perhaps some CALM, deep breaths or inwardly tell your heart to be quiet and listen to it obeying you.
Thank you TS, for your thoughts.
To “try not to” or to “tell my heart” is like talking to a dumb beast. I have gently asked my heart to be quiet. I can almost stand aside and watch myself being in a stressful situation. It seems my body is an independent entity and it will do what it will do. TM training, mindfulness, regular exercise all notwithstanding, “he” does what he will. Sounds dissociative maybe? Feels that way sometimes.
Perhaps it’s my vegus nerve with the independent agenda?
JD, I don’t want to cross the line into specific medical advice (especially because I work primarily with children), but I can say that I’ve had a number of children and adolescents who have only been able to learn from deep breathing, CBT, mindfulness, etc. and develop coping skills after treatment with an anti-anxiety meds (due to the severity of their condition). I’m not a medical provider, so that part is always done via referral, but my experience has been that a debilitating anxiety sometimes has to be treated first via meds. (I saw your comment above about beta blockers, but there might be help for you down another avenue.) Once the body is calm, the mind is more receptive to other experiential treatments.
KidPsych,
Thanks. Uh . . . another avenue? Hint?
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1182327/
Abstract
Summary
There is increasing concern that most current published research findings are false. The probability that a research claim is true may depend on study power and bias, the number of other studies on the same question, and, importantly, the ratio of true to no relationships among the relationships probed in each scientific field. In this framework, a research finding is less likely to be true when the studies conducted in a field are smaller; when effect sizes are smaller; when there is a greater number and lesser preselection of tested relationships; where there is greater flexibility in designs, definitions, outcomes, and analytical modes; when there is greater financial and other interest and prejudice; and when more teams are involved in a scientific field in chase of statistical significance. Simulations show that for most study designs and settings, it is more likely for a research claim to be false than true. Moreover, for many current scientific fields, claimed research findings may often be simply accurate measures of the prevailing bias. In this essay, I discuss the implications of these problems for the conduct and interpretation of research.
Someone once said, “Truth is like poetry. Most people hate it.”
May/June 2012
Something Doesn’t Add Up
Too much medicine relies on fatally flawed research. Epidemiologist John P.A. Ioannidis leads the charge to ensure health care you can count on.
By Joan O’Connell Hamilton
Last June, Stanford orthopedic surgeon Eugene Carragee and his editorial team at the Spine Journal announced they had examined data that Medtronic Inc. presented a decade ago to get approval for the spinal bone graft product sold as Infuse.
Not only did the team find that evidence for Infuse’s benefits over existing alternatives for most patients was questionable; they also discovered in a broad array of published research that risks of complications (including cancer, male sterility and other serious side effects) appeared to be 10 to 50 times higher than 13 industry-sponsored studies had shown. And they learned that authors of the early studies that found no complications had been paid between $1 million and $23 million annually by the company for consulting, royalties and other compensation. Carragee, MD ’82, estimates Medtronic has sold several billion dollars’ worth of Infuse for uses both approved and “off label.” Medtronic issued a statement saying it believed the product was safe for approved use and gave a $2.5 million grant to Yale University researchers to review the data. Their analysis is expected this year.
The financial influence Carragee’s team unearthed makes this case particularly jarring. Yet the phenomenon of flawed research is not new. Medical science studies routinely reverse or cast doubt on previous research that guided physicians’ recommendations on everything from which fat we can safely slather on our morning muffin to some of the most invasive and expensive procedures doctors perform on the human body. No wonder many people feel less than confident when facing important health decisions. If it seems that the pace of these contradictory reports is picking up, it’s not your imagination.
Prompted by soaring health-care costs and increasingly sophisticated analytical tools, more and more medical treatments are taking their turn under the microscope. One driving force is John P.A. Ioannidis, chief of the Stanford Prevention Research Center. He works with colleagues around the globe to scrutinize treatments that account for huge chunks of the health- care tab but that are, he says, virtually worthless and sometimes harmful. Ioannidis says financial influence is one of several factors that can, deliberately or unintentionally, skew study design and methodology and undermine the validity of published research findings. His extensive publications pointing out these problems are reverberating throughout the scientific community—and threaten entire medical specialties that have organized themselves around big-ticket, but low-value, interventions.
“Fixing this involves a rethinking of the process that won’t happen overnight and is not very cheap,” Ioannidis says. “However, if we continue in the same path we will run out of money, as a country, even the whole world . . . there is a cloud of ineffective interventions, or minimally effective interventions that are extremely expensive and therefore not worth it. We need to sort out that mess.”…………
continued here
https://alumni.stanford.edu/get/page/magazine/article/?article_id=53345
Hi Mr Chris
Re. your additional comment:
I’ve just re-read my comments on hs-crp test and I was sure I typed in all the ranges but they haven’t appeared: Here they are:
3.0 – 10.0 mg/l = higher relative cardiovascular risk
Your reading was less one so low relative risk.
However…
I gather this is just one of several tests for cardiovascular risk. For example, you may wish to read Dr Kendrick’s blog on diet and the various comments on vitamin C deficiency and lipoprotein (a), also known as the Unified Theory of Cardio Vascular Disease. You can test your lipoprotein (a) levels and that’s another possible risk assessed. Some of the commenters provided links to this and also on the sort of inflammation risk tests you can do such as hs-crp, lipoprotein (a) and homocysteine.
My near fatal CV event was in April with no known cause so I’m on a learning curve and trying to find out what happened, if possible. That’s where I’m coming from – feel like I’m walking around holding a ticking bomb. Hopefully, getting these tests done will either give some peace of mind or allow me to monitor what’s going on based on all the current hypotheses.
Regards
“My near fatal CV event was in April with no known cause so I’m on a learning curve and trying to find out what happened, if possible. That’s where I’m coming from – feel like I’m walking around holding a ticking bomb.”
Happened to me 17 years ago.
My advice is to escape the “health care system” by all means and take control of your own health without any medication and cutting, i.e. do your homework and turn into an expert in your own “disease”.
Hello Göran
I do agree with you. I have learnt many things here, perhaps the most important is to think for yourself, be in charge of your health, and read read read about your alleged condition. In the end you are probably the expert.
What you say about Chalmers makes me wonder if it isn’t a stress factory.
Well, then. Let us look into the interactions of insulin, grehlin, leptin and glucagon. In my online researches yesterday, I was given to understand that we have a resting insulin level. Never thought of that. A resting insulin level can be low or high. Obese people have a higher resting insulin level. It’s my understanding that much of the damage in metabolic syndrome is done by insulin, such as raising blood pressure, and I believe that somewhere upthread there was commentary to the effect that damage is being done to the micro capillaries early in the game, not late. So if that is true, it means that the people who are able to keep their blood sugar normal, like me, but who have high blood pressure, a bit of fat, and a Hgb a1C of 6.0, (norm is below 5.7 for you Brits) are probably struggling. Could that be why the eye doctor said I have early signs of cataract or why I have a middle toe that sometimes goes a bit numb? I have recently heard Alzheimer’s being called Diabetes of the Brain. To be sure, senile dementia is probably a big area, what with the brain being so complex and all, but it could be true for a portion of people. What if some of us never manifest overt diabetes but instead succumb to Alzheimer’s and CVD? It would answer some questions. When you see a guy with a big gut you think metabolic syndrome but maybe he tests negative. So an early manifestation of problems would be to do a fasting insulin test, not a fasting glucose test which may show up high 20 or more years later.
Higher insulin levels make it very hard to lose weight. Fasting apparently resets it lower. So this intermittent fasting may be an important key. Perhaps people who cannot tolerate any carbs would be able to if they fasted occasionally.
This ties in with my earlier puzzlement over the fatness of Americans and their kids. I think that constant snacking has become the norm, as well as not putting children to bed early enough and eating after dinner. Never going more than a couple of hours without food plus the low quality of much of what gets eaten is probably key here to never letting the body rest from insulin. I once read that the French do not eat between meals.
I know glucagon is a lifesaver, but most of us never put it to work!
As for grehlin and leptin, we need to see how we are stimulating the one or the other. (These are the satiety and hunger hormones.) So far, after a few minutes of googling, the results seem counterintuitive. Fat cells inhibit appetite and insulin inhibits the hunger hormone.
Chronically raised insulin inhibits hormone sensitive lipase – preventing us from using our fat stores – and makes us crave more food.
Anna, how do you know that your blood sugar is normal? Is it based on a glucose blood test after a 12 hour fast? If so, that is a useless test IMO. If your HbA1C is 6.0, that is already high in my book and indicates that glucose is hanging around in you circulation for longer than desirable. That also means that your insulin levels are probably higher than baseline for longer than 3 hours. Normal people should get their insulin and glucose back to baseline in less than 3 hours after a meal. (Do a search on work done by Dr. Kraft). Also, the fact that you have “a bit of fat” and higher than desirable blood pressure (over 135 mm perhaps) would indicate that you might already be on your way to T2 diabetes. Try going on a very low carb diet and see what it does for you. Eat as much animal fat and saturated vegetable fat as you want. There is no such thing as an essential carb, so you don’t need to eat any for good health. Glucagon and the liver will take care of any glucose needs you may have.
Saturated vegetable fat?
I have not really checked a post meal blood sugar. I ought to. I only have a couple of morning tests. Of course my sugar is higher than it ought to be. As far as I am concerned, being in the prediabetic range really means that I have diabetes, but in early stages. The 6.0 means my sugars on average are too high.
I have backslid on an earlier attempt to go low carb. Now I’m back to it. I find it easy to go 16 hours without eating, and so I eat 2 meals a day. Now I’m going to be much stricter with the low carb and no snacking, although most days I don’t. Still, I find it troubling that I should not be able to eat potatoes, which I grow in my garden, or squash which I grow for the winter. Something seems wrong about all this.
My solution is to eat 2 meals, and one of them will be non carb, then one meal when I will include good carbs. I may also do some fasting in which I eat one meal per day.One guy on youtube said a 24 hour fast resets the insulin level lower. I get really hungry after that!
Don’t worry, I eat a very high fat diet. This annoys me too, though, as I have been eating high quality fats, raw butter and cream, coconut oil, lard, etc and it hasn’t done me as much good as I might have expected.
Anna
It also may be that “low carb high fat” is not for you. I warned here before. You might reconsider your approach.
What did you say in your warning?
I said that people on “low carb” diets often remove “evil carbohydrate” foods that are, unfortunately, very good sources of fiber (complex polysaccharides that serve as food for our gut flora) and various micronutrients, such as magnesium, copper, manganese, boron etc. These food include whole grains, seeds, tubers, fruits… Micronutrient deficiencies are detrimental for health and impair regenerative processes.
Thanks. I’m not a fan of modern grains but I take your point.
‘Over 135 mm’ really, well that’s a lot of people over 60 going to the knackers yard then.
I wonder why some young mums are constantly putting food into their tots mouths, wherever I travel, buses especially, now I have my bus pass, there they are little one in buggy, mum feeding open mouths, don’t they sit down and have breakfast before leaving home. It happens in my family too, can’t stand it. Sit at the table for meals, not in front of tele. This constant snacking and drinks on the go, should be illegal. My age I guess, war baby.
‘I know glucagon is a lifesaver, but most of us never put it to work!’
Nothing much appart from removal of the pancreatic alpha cells or various rare pathological conditions seems to slow down glucagon production capacity. However the intricate dance of insulin glucagon somatostatin leptin and etc. is astoundingly complex since they all influence each other and it often progresses counterintuitively. Sorry, it ALWAYS progresses counterintuitively.
Insulin and glucagon not only regulate blood sugar, they also control protein and fat disposition. The typical view is that insulin is broadly anabolic and glucagon catabolic. One builds, the other pulls appart and I supppose that just as excess use of anabolic steroids can lead to cvd-chd then so can excess insulin.
Persistent hyperglycaemia is usually due to excess glucagon action wrt insulin. Either insulin is insufficient or glucagon production is not properly inhibited by insulin. Glucagon is stimulated by blood sugar just as insulin is but is then down regulated by counterveiling spikes of insulin. In the absence of inhibition by insulin, glucagon production is both driven by blood sugar levels and also drives them higher. Perhaps better to avoid provoking it in the first place?
Hypoglycaemia is usually only caused by excess insulin or insulin sensitivity. As far as i know, type 1 diabetics will only get absolute hypoglycaemia if they take too much insulin. Under otherwise normal circumstances, their glucagon is mostly uninhibited and while energy stores remain, glucose production will take place and excessive ketone production and so on.
Reactive hypoglycaemia is a different matter. Anyone can experience that if their blood sugar drops rapidly even if it doesn’t descend to pathological levels. The brain ‘panics’ because it can’t adapt quickly enough, or maybe not just the brain but lots of other cells too = a hormonal crisis.
The term ‘insulin resistance’ is tossed around pretty lightly and frequently abused. There are several types of insulin resistance to be teased apppart and eg in the context of chronic hyperglycaemia many cell types will simply wind back their insulin sensitivity to avoid catastrophic overload eg glucose transporters will be down regulated or insulin receptors ditto. It is normal and healthy regulation. But that ain’t the whole story.
There is very much the smell of a chicken-egg situation about all of this. Alzheimers and some other types of dementia are now described as another type of diabetes or energy supply problem and are frequently associated with depression. On the other hand untreated type 2 diabetes directly causes memory loss and depression and various other problems like that but these are generally reversible or controllable by eating properly, excercising a little and taking appropriate pharmaceuticals.
A car needs to have its computers (driver, electronic) in good order but also a healthy battery and charging system, and a power plant being fed the right type of fuel in order to continue functioning. Without the very specific correct fuel it doesn’t matter what the brains say the car will not run, the battery will also go flat and everything will grind to a halt. People are much more adaptable than cars but the same general principles apply.
Craig
Persistent hyperglycaemia is usually due to excess glucagon action wrt insulin. Either insulin is insufficient or glucagon production is not properly inhibited by insulin. Glucagon is stimulated by blood sugar just as insulin is but is then down regulated by counterveiling spikes of insulin. In the absence of inhibition by insulin, glucagon production is both driven by blood sugar levels and also drives them higher. Perhaps better to avoid provoking it in the first place?
Seems to me that it is necessary to measure both and possibly leptin and to establish the real “cause” of T2D; all of which are studiously ignored by the NHS as pointed out by Dr Kendrick above. Persistent hyperglycaemia is what affects me despite 24-36 hours fasting.
Do you have a reference on the subject that I can fire at the NHS intelligentsia?
Mike I have that info from a range of sources and I will dig out some refs for you. It’s worth noting that protein also stimulates glucagon and insulin. Dr. Bernstein says to measure protein intake when calculating insulin for t1dm, and several low carb gurus suggest keeping protein intake moderate.
Some proteins more so than others.
There are gastrointestinal alpha cells as well as pancreatic which might one reason that bariatric surgery can stop t2d in its tracks. At a huge cost of course.
Mike,
try some of the refs that George Henderson gives here:
http://hopefulgeranium.blogspot.com.au/search/label/Diabetes%20question%202?m=0
And the other work of Dr Roger Unger, eg
http://www.ncbi.nlm.nih.gov/pubmed/4436439
I would like to draw your attention to a paper co-authored by Dr Kendrick in the BMJ Open. The link is :
http://bmjopen.bmj.com/content/6/6/e010401.full.pdf+html
There are some rapid responses on
http://bmjopen.bmj.com/content/6/6/e010401/reply#bmjopen_el_9955
One reference annoyed me because it cited the benefit to the elderly as 39.4%(a relative rate) for MI (no death) and a 23.8% reduction in stroke (not death) but while in Table 2 It is clear that all cause reduction in DEATH was insignificant at <1 in a 1000. from statin use.
Yes, statins do have a trivial probability of benefit but the 39.4% decrease in MI was in real terms about 1.5% (or only 1 in 67 would benefit) while stroke at 23.8% while the real benefit was only 1.1% (only 1 in 91 would actually benefit).
This is an example of a 25 to 40 times of inflation of the real benefit. WHY? The only reason I can think of is to flog drugs.
The probability of statin use benefiting the individual patient in preventing an event is simply trivial but there is an even lesser chance of surviving. The HPS study post-MI results suggesting about 0.3% survival per year.
And then these meta-analyses depend on "SELECTION" of studies. This in itself can massively bias studies. Expert Rev. Clin. Pharmacol. Early online, 1–10 (2015) by David M Diamond*
and Uffe Ravnskov makes this point.
Dr. Kendrick,
I just finished reading the Great Cholesterol Con, and just today finished your heart disease series of blog posts. fascinating and thought-provoking stuff. I’m 55, normal weight, fit male, feeling better than I have in years (eating well, exersizing, and sleeping well). Problem is, my LDL is through the roof (not as high as heterozygous FH, but pretty darn high) and my doctor is REALLY pressuring me to go on statins – which i have refused so far. I don’t smoke, don’t take any prescriptions, and my HDL is great, my trigs are super low and my BP is perfect. yet my doctor insists I’m a dead man walking. My question: in a future blog post, could you adress the issue of plaque “healing”? I apparently have 50% blockage in my carotid arteries (ultrasound results) and I’m wondering if a proper lifestyle of real food, stress management etc will slowly undo the damage. Up until my early 50s I ate like a fool (standard american diet), ran too much and had too much stress, so I’m pretty sure those are the years that I formed the plaque. If I had the hope that i could heal my plaque, even over many many years, I would take that option over statins. If i understand your theory correctly, I need the rate of plaque “healing” to be greater than the rate of endothelial damage and new plaque formation. I would really appreciate some info on how plaque can recede or diminish, what the mechanism is for that. Dr. Steven Masley (cardiologist) claims to have successful plaque reduction in his patients, so unless he’s lying, it must be possible. And if anyone has scrolled down far enough to read this and can point me in the direction of any internet resources on this topic, i would really appreciate it!
Dan
I wonder though, if in my case stress might be the cause of some of this. In my case, mostly job stress. On that note, I can say that has recently improved greatly, but it went on for years.
I have read that following the collapse of the Soviet Union alcohol consumption in East Europe fell by 7% over the next decade. So there is a clear association with your graphs showing the rise of CVD in Lithuania and Latvia in the same period. Before retiring I often had highly stressed days and found that stopping on the way home for a pint or two was a great stress reliever. Is this a causal relationship? Discuss
I doubt that 7% decline in alcohol consumption is what accounted for higher CVD rates in Lithuania.
Stress and strain and ad hominem attacks (it’s not just the professionals who get them)
Hi Goran and Mr Chris (and all readers I guess),
Very excellent and timely advice about escaping the healthcare system and taking charge of yourself. Read about my long awaited apppointment with my NHS cardiologist and my long, long list of questions…
…to which she replied, we’ve only got a few minutes so let me do my stuff and if we have time we’ll get to your list.
Medication (I’m on 6 medications and hoping for reductions) – nope, we’re not dropping any and increasing the dosages for some. I mentioned polypharmacy which drew a blank and she stated several times that this was keeping me alive and was for life. Oh dear.
I knew where we stood now – NHS/NICE guidelines and no variance.
I mentioned blood tests for monitoring cholesterol, inflammation and was told it was a waste of time and NHS money and to keep taking the medications. I thought it reasonable that if you insist on shovelling bags of medication down my throat, I’d like to know what’s going on. Go private then and if you are unhappy with UK healthcare, go and live elsewhere. No joke – that’s what she said.
I frittered away my final few seconds cos I knew the answer – had she heard of cardiologist Dr Aseem Malhotra? She had (that’s good news I thought) but, predicatably, he was a pariah, controversial and wrong – no surprise there then.
The ad hominem attack? Having dared stick my head above the battlements, she said I was very angry (I was when I left) and would write to my GP recommending I get some psychiatric, professional help.
Couldn’t believe my ears.
That’s was my 5 mins.
As reader of this blog will recognise, my summation of this 5 mins met with familiar tactics, a bit of bullying (caridologist is right – do as I say or you’ll die), a variation on the killing of lives (mine) and a personal insult that I needed help for mental health issues.
I’m pretty scared about the medication situation but I have been learning so much from everyone here and all Dr K’s blogs going back to 2012 and will take control.
On that note better go and find a private lab for my blood tests.
Regards
I have no advice, just sympathy. The Dr cncerned needs help with their narcissistic control issues.
Wow…
I am appalled that any doctor would treat patients with such distain and temerity.
Charles, Frederica
I too find the behaviour of the cardiologist appalling. She gives fives minutes, is not interested in discussion or explaining, and finishes by implying you are crazy. Did she tell you what and why she is treating you? Take the package leaflets of your six medicines and study them including side effects. I would suggest putting them into the Kendrick search function.
Finally if you do decide to consult privately do not go to her.
1984 has finally arrived.
Charles Gale
You have my sympathy too.
NHS/NICE guidelines and no variance.
My general complaint about guidelines is that they are usually written in the main by conflicted “experts” who are only concerned about the HERD and flawed statistics based on “selected” studies that support their beliefs. Then one has QoF (Quality of Outcome Framework) which appears to have been designed to control GPs and ensure that they abide by the guidelines. They certainly have not been designed for the individual patient; for example I have been assured that QoF contains no section for adverse reactions to drugs. This is compounded by consultants devoid of individual thought as you have found.
This attitude always reminds me of the Polderman guidelines on beta-blockers and the consequent 800,000 deaths (the study that estimated this figure was taken down for review and never seen again) but Polderman was sacked from his job and the chairmanship of the EU committee that produced the guideline.
Now well into my ninth decade I depend on my GP, nurses and indeed consultants in the local NHS hospital – not on the drug flogging experts of the medical establishment. So far they have served me well!
May I suggest that many commentators on this blog are well able to take advantage of the BMJ’s Rapid Response system to present a patients view or even apply to be a patient reviewer.
Quote from Medical Daily 2015:
‘One of the most common questions people ask health care providers is, “Can I use my old drugs past their expiration dates?”
Though expired medications retain their potency, no scientific study has ever tested and verified the safety of expired drugs in humans. (Reuters)’
I think we can guess why pharmaceutical companies would not want to fund or encourage such a study. So poor, foolish health services will continue to be ripped off. It might pay them to do their own studies. I’m sure there would be willing volunteer taxpayers for subjects – especially in the paying USA where expired drugs could be given free of charge to willing, appropriate subjects.
Never mind all the intact, in date drugs that “have to be” destroyed. What a despicable nonsense. So frightened of litigation that reason has flown or another example of revolting greed ruling?
http://www.medicaldaily.com/what-your-pharmacist-cant-tell-you-about-drug-expiration-dates-its-complicated-342978
The US army once did a study on their old stocks of aspirin. 13 years on they were still effective.
On the other hand the way drugs are stored, whether tablets, liquids or gels will affect their survival, Tablets in their single sealed “cards” will probably survive and kept at a low temperature will survive best.
The drug companies are required to put their products through rigorous “environmental” tests to determine shelf live but in the “interests of safety” the expiry date will be set as short as allowed.
I am afraid that I tend to ignore expiry dates on the grounds that “safety” is probably more likely to be related to BP protection than patient protection.
Thanks for the comments on my cardiologist appointment this morning.
Never noticed the search function on Dr K’s website – thanks for pointing it out.
I’ve been catching up on Dr K’s blogs dating back to 2012 when it started and a common theme is the exasperation expressed by readers of this blog is that these educated, trained, intelligent healthcare professionals cannot either conceive or consider any other hypotheses beyond the lipid hypothesis, or whatever the NICE guidelines state.
I’ve read the answers such as money and some great observations/quotes from readers and experts about why but today’s encounter still has me baffled, sad and exasperated. But since my collapse I’ve dealt with 2 GPs, an endocrinologist and a cardiologist. No matter what you say, what books you bring, printouts, it was like smashing your head against a brick wall. I note that none of these 4 had anything to offer despite criticism – no research, don’t appear to have published or done anything…my endocrinoligist actually said she didn’t have time to read anymore.
What also saddened me this morning was the cardiologist stating that she wanted to increase some of the dosages but had done no testing on me (beyond weighing me and taking my blood pressure) nor enquired about any side effects before making her decision. Surely, if you are going to for example insist on statins, don’t you want to know what’s happened to my total cholestrol levels since my last blood test? Or check my insides?
Rant over!
Charles,
I am today very convinced that most medical experts belong to a criminal organisation but at the same time are the last to admit this “scientific fact”. For these experts consensus is science but not for people thinking deeply about the theory of scientific knowledge. The GP’s are more “innocent” to my opinion.
My last cardiologist was actually the most aggressive representative of the medical profession I have ever come across but his aggressiveness was quite understandable since I had already been challenging his world for 15 years when I met him two years ago and he was more than aware of this fact. When specifically asked if he was surprised about my “reasonable” health status he went silent for a short while but then blurted: “You have only been lucky!”
So this is the much vaunted single payer government healthcare that all of us Yankee’s have been hearing about huh? We have our share of quacks in the States. But at least we get 15 minutes with them in most appointments!
A Man
I thought the UK rule was fifteen minutes one symptome?
Whatever, no blood tests cause they cost too much!!!
Not really a pofessional
Man, the NHS is often good, but far from perfect, particularly in the areas of most interest to this website. However, the US spends twice the amount of GDP on health and many working citizens seem to spend their lives worrying about health insurance. My American friends don’t recommend their system to me.
Please. US healthcare system is probably the worst in the developed world. The only reason they don’t fix it, IMO, is because eliminating all that waste and fraud would tank US economy.
A Man
Officially according a surgery notice it is 10 minutes. On the other hand since it costs nothing how many appointments could be dealt with by the practice nurse or the local pharmacist. Unfortunately a “free” service can be abused; it seems that a proportion of the population in the UK is quite prepared to abuse the system. As an example I once asked a shelf stacker in a large national supermarket store where the aspirin (costing about 20p) was to be found. Her answer was that I should go to the doctor and get a prescription to get it free. I leave it to readers to guess my response.
From what I’ve seen, things in the U.S. started going downhill with the invention of health insurance in the 1950s. Now my 90-year-old friends are getting moles slashed off their faces because they are told they may develop into skin cancer, and every Medicare-eligible soul knows what he is “entitled to” as far as services go per year. (They stop the service as soon as the limit is reached, showing that they really do not need the service.) If people paid for their own doctors’ visits and their own prescriptions the amount spent would plummet and probably people would feel better because they would not be agonizing over the medical “issues” that they only learn about from the test results.
I am 78 and have not had a physical exam since my 20s, when my children were born. I do not know my blood pressure and have never had my cholesterol levels tested, and I feel just great. When I needed medical attention after fracturing a wrist I had a wonderful experience in the emergency room of the local hospital and with the talented surgeon – a specialist in hand surgery – who set my wrist within three hours of the accident. The total cost of the treatment paid for by my company’s insurance company was about $7,000. Over the 25+ years that I worked, for which my employer paid over $1,000/month for me and my husband, that was the only expenditure that I incurred. I would have been much better off if I could have had that insurance money as part of my paycheck and been responsible for paying my own costs, but that was not allowed by my employer. The farther away the patient is from the actual cost, the higher the costs will rise. Just think of how much money health insurance administration costs! People should be able to take out real insurance, covering costs of over $25,000/year, as an example, and pay for incidental visits as they arise. Such insurance is no longer available in the U.S. as the government is “helping us” by forcing insurance companies to cover abortions and maternity care, for example. The U.S. government now penalizes us if we do not need or want health insurance, all in the name of making it “affordable.” What a ridiculous situation!
And what a ridiculous attitude.
The answer is cognitive dissonance. Has been afflicting the medical profession since time immemorial.
Charles,
I think you have every right to “rant”. As a patient I am very keen on patients ranting particularly in medical journals such as the BMJ were patient comments are excepted under the Rapid Response system.
No matter what you say, what books you bring, printouts, it was like smashing your head against a brick wall.
Not all but some. I think your endocrinologist sums it up very well – no time to read; no time to report adverse reactions, (an option rather than mandatory) and excluded from QoF (Qualityof Outcome Framework) but very important to patients but challenges BP profits and status of their KOLs (key opinion leaders) along with a recent paper in the BMJ (May – estimating US deaths at 250,000 pa) http://www.bmj.com/content/353/bmj.i2139 This confirms the findings of by Starbridge (2002) who reports Total deaths = 225,000/year of which 106,000 were attributed to properly prescribed and properly used drugs (JAMA, July 26, 2000—Vol 284, No. 4 483) and a more detailed estimate of over 750,000 by Null and Dean (Journal of Orthomolecular Medicine Vol. 20, No. 1, 2005). This paper is based on reports published in many prestigious general and technical medical journals and official US government reports. There are no similar reports for the UK but as both systems use similar drugs and guidelines it is reasonable, in the absence of data, to assume a pro-rata result which leads to some 40,000 deaths in the UK from medical error and drug associated deaths.
What scares me is the apparent indifference of the NHS and the medical establishment to this situation and their proclivity to “hide” these facts. May I suggest some useful books that show these problems. Dr Kendrick’s “Doctoring Data is probably well known; Dr Marcia Angell’s (ex-editor-in-chief of the NEJM) The Truth about Drug Companies……………..; Professor Gøtzsche’s Deadly Medicines and Corporate Crime (a BMJ prize winning book) for starters. I also found Dr LeFanu’s The Rise and Fall of Modern Medicine a most interesting and insightful book – well worth reading. In short there are doctors out there who are very concerned about the aberrations of the official medical administration and patients should try and support them. Theoretically the Hippocratic view is to help individual patients; it has nothing to do with the “herd” or statistics. For example when reporting an adverse reaction, to be told it is very rare when for the individual it is 100% is simply very irritating.
I would also recommend books by Dr Welch (?sp). “Should I be tested for cancer? Probably not and here’s why” and others by him.
Diana,
When I first tried low carb high fat a year or so ago, I did have a decrease in blood pressure. As for the food categories you mentioned, I eat a lot of vegetables, eat quite a lot of nuts and seeds, fruit mostly in season. I wonder what you think I should be doing if not decreasing carbs, with a high average blood sugar? Perhaps if I went vegan, since that is a semi starvation diet and many are thin.
Anna
I cannot tell you what you should be doing because I do not know you. What exactly are your issues? High blood pressure, high blood sugar, a bit overweight? I tried to tell you that the “go low carb and eat high fat and your problems will be solved” advice may be totally wrong in your case, for the reasons mentioned above.
My general tip no. 1 would be up the fiber – you may not be getting enough at all – from real whole plant foods, yes potatoes included, why not, especially when you grow your own?
Complex polysaccharides (= fiber) are fermented by gut flora into various metabolites such as SCFAs (short chain fatty acids) that have been shown to bind receptors in the body regulating so many other processes, including blood pressure and blood sugar regulation. See for instance:
“A novel SCFA receptor, the microbiota, and blood pressure regulation” (Pluznick, 2013)
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4063845/
For more information about feeding your microbiome read for instance papers or books by Justin Sonnenburg. Or read “The Potato Hack” – weight loss, improved blood sugar regulation…. or here a paper:
“Intestinal Short Chain Fatty Acids and their Link with Diet and Human Health” (2016)
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4756104/
Hi Goran
Always enjoy reading your comments and I imagine myself and probably other readers/visitors to Dr K’s website are treading the path you walked 17 years ago concerning healthcare professionals and taking control of one’s own health.
If you have the time/energy/interest, would you mind briefly telling me how you went about it? I left hospital with a stent, cardiac implant device in my chest and 6 medications to take for life. And i’m now considering what to do about all this.
Is that a familiar scenario? Did you do cold turkey? Was it a gradual, cautious reduction over the years? Regular blood checks to monitor your progress? If you were stented and implanted, did you ever have these things removed?
Hope you don’t think this is too personal. I wouldn’t consider it as advice at all – maybe general answers. I’m very curious.
Regards
Charles,
I really don’t mind telling my “story”.
1. Before my emergency trip 1999 I firmly believed that the medical business was some kind of natural science as I was familiar with from my metallurgy research. Today I see just religious dogmas.
2. I was evidently very “close” according to the “experts” who didn’t understand why I had survived the attack except for the collaterals.
3. The angiography revealed that all coronary arteries were “clogged” and there was no use considering stents. I was therefore offered a “complete” by-pass which I declined after having done my “home work”.
4. Being a “believer” 1999 I did not refuse the five drugs offered though not any statins since my cholesterol was “so low”.
5. Doing more of home work I realised that the medication wouldn’t solve any problems and be contra productive in the long run and that I had to do something about the “cause” in the broad sense.
– Cut all medication – after a year and most in half a year
– Cut all sweet stuff – immediately
– Cut all “partially saturated vegetable oil” – read margarine – immediately – eat butter
– Introduction of regular low grade exercise – took my bike to work every day (12 km one way)
– Found a new less stressful job
6. For ten year everything was then fine until my wife realised she was seriously diabetic
– We then decided to cut “all carbs” (as far as this is practically possible) and experienced dramatic health improvements on IBS, night vision, peripheral neropathy and as a bonus normalised our weight (- 20, -12 kg respectively).
7. Now with 7 years on the “tough” LCHF trail it still feels pretty fine
Lessoned learned. “Do your homework an keep away from the health care system at all cost – they will kill you sooner or later if the get the chance and for sure make a nice profit on the business.”
See this obesity map of the USA—–
http://www.bantransfats.com/obesitymap.html
Errett
An excellent Link many thanks.
One would have thought that such a series of graphs would make even the most convinced expert to start re-thinking the problem.
Hi Mike (Cawdrey) and Goran
Many thanks for the time put into your comments on how the healthcare system works/doesn’t work and for your “story” Goran. Put together you both sum up the frustration (and reasons why I’ve ended up battering against this brick wall) of the last 4 months in my life to try to find causes.
Plenty to think about going forward and feeling more empowered the more time I spend on this website.
Thanks again!
Re Anna’s post of Aug. 30 and further posts and comments by Bob and Diana
Bob,
Your point about Hormone Sensitive Lipase is very important, and most folks are not aware of this hormone. Permit me to expand a little. HSL is active in mobilizing your fat cells to drive Lipolysis (breakdown trigs and transfer fatty acids to the circulation). That is how we remove fat from our fat cells. HSL and therefore Lipolysis is suppressed by high insulin levels so when your insulin level remains higher than baseline, your fat cells are not generating any fatty acids to provide nourishment to all your other cells. And if your circulation is devoid of any glucose (or ketone bodies), your cells will be starving and your brain will send you a message to eat something. (You will feel hungry, as you said). If that something you choose to eat is carbs, your body will be happy immediately, but later the cycle will start again. That is (one way) how we gain weight, slowly but surely. High insulin level for a longer than normal time drives weight gain through hunger.
Now the reality is that we need to “adapt” our body to not rely on carbs as the main form of nourishment if we wish to get our fat levels down. This requires (according to Drs. Volek and Phinney – see their book and research studies) about 2 to 3 weeks of NOT eating carbs in any significant quantity, preferably less than 20 g per day. That is also why Dr. Atkins imposed the induction period into his recommended diet.
Anna, if you flip flop from low carbs to substantial carbs within the same day, you will never adapt your body to burn fat. This is crucial. Yes, you may be fine eating some carbs after a period of adaptation, but it is very important to break this dependence.
Diana, Anna may indeed not be fine on a low carb way of eating, but the vast majority of people do respond very positively. What is really important is to measure – your glucose levels, your HbA1C, your blood pressure, and anything else that may be relevant. It is not carbs that are “bad”, it is what our body does with them that is significant (insulin resistance). So eating potatoes and fruit may be ok for most people who can tolerate carbs well (such as most of us when we were young), but some of these macronutrients end up as glucose in your circulation (and some as SCFA’s as you mentioned). They are less “harmful” than sugar and wheat, but for someone who is sensitive to carbs and exhibits a high HbA1C and admittedly high blood glucose levels, it seems to me that the first course of action should be to reduce carbs to a minimum (< 20 g/day) for a 2 to 3 week period and see how the blood markers behave. Most people report great satisfaction, improved blood markers, and greater energy levels than before. One can try going back to some carbs later, although I don't agree with your position that these macronutrients are as important as you make them sound. There are other options which do not include carbs. Anna is exhibiting the usual signs of lack of insulin sensitivity. More carbs is not the answer to this problem.
Bob, sorry about the "saturated vegetable fats". I was meaning to refer to fats derived from vegetation (such as Olive, Coconut, Palm, and Avocado oils primarily). Yes, they are fruits but not everyone recognizes this point.
John U
I definitely do not agree with your view. Do you call fiber a “macronutrient”? And I have also mentioned micronutrients…. how do these fit into your “story” and “teaching” of the people you recommend to read?
I definitely do not dare to diagnose Anna based on the little information she gave. But I have warned her.
The main point is that “low carb high fat” diet has no evolutionary example in human nutrition.
It has virtually the whole of human history. But, as Fung points out, it isn’t just the carbs.
‘The main point is that “low carb high fat” diet has no evolutionary example in human nutrition.’
???
Sorry, I don’t like to distract from the main discussion but I am evolutionary and I eat like that, and:
https://en.m.wikipedia.org/wiki/Head-Smashed-In_Buffalo_Jump
http://www.sciencemag.org/news/2016/01/grisly-find-suggests-humans-inhabited-arctic-45000-years-ago
Innuit: ‘The fat, not the protein, from animal foods provided most of the 3,100 calories required daily for these active people’
Plus countless other examples.’nuff said.
I find it slightly amusing that even though Malcolm explained in his previous blog, why he doesn’t think diet is a major factor in causing CVD, the arguments about diet continue without even much reference to the idea that this may not be relevant, or at least not as relevant as many here seem to think!
Admittedly there is the issue of diet causing T2D (which in turn causes CVD), and that makes me lean on the side of avoiding too many carbs, but we surely have to face that fact that people are omnivores, and eat a wide variety of diets. You couldn’t feed a cat (for long) on vegetables, and you couldn’t feed a rabbit on meat, but because we are omnivores, we can consume both types of food!
The official medical advice seems stuck in a groove, but the discussions here also seem just as stuck in a slightly different groove! If the main cause of CVD is stress, then all this talk of diet is basically irrelevant.
We can, but should we? Some might find it amusing that you and the good Dr have both felt the need to talk about diet and are clearly on the same page – or at least readingwthe same book – as low carbers. I’ll remind readers once again of Dr Kendrick’s two part piece on what carbs do to you.
David
I am reading this blog because the question “What causes…?” sounded intriguing enough.
I research plant microbiome and know nothing much about CVD, only searching common points related to the health and disease of organisms. Plant-microbiome relationship often parallels human-microbiome relationship. For instance, plant microbes mediate/moderate both biotic and abiotic stress the plant is exposed too. I doubt humans are much different. The link nutrition – microbiome is hopefully clear. Here a paper suggesting a link between stress and (healthy) microbiome of animals:
“Link between stress, unhealthy microbiomes discovered” (2016)
https://www.sciencedaily.com/releases/2016/01/160106091735.htm
“Red squirrels living in a low-stress environment harbor healthier communities of micro-organisms, a result that might hold implications for human health, according to a new study. “
Diana,
“Do you call fiber a “macronutrient”? And I have also mentioned micronutrients…. how do these fit into your “story” and “teaching” of the people you recommend to read?”
I do not call fiber a macronutrient. I was referring to starches and fruits. Sorry if there was confusion. Regarding micronutrients ( and fiber), I have abstained from commenting on these. There is no question that they are important, but I personally believe that I obtain enough in my normal diet. If I think that I don’t, I will supplement. I think that if we wish to offer advice, we should concentrate on those issues which are most important at the time, and I think that micronutrients and MCFA produced in the gut are not the main issue here. High glucose levels for a longer than ideal time period are. Furthermore, what I am suggesting is not in any way harmful. I, and many, many others have eaten like this for years.
“The main point is that “low carb high fat” diet has no evolutionary example in human nutrition.”
I would have thought that hunters and gatherers ate mainly a HFLC diet. Certainly there is plenty of evidence of migrating tribes of N.A. natives eating pemmican, during their migrations, something that they would do for months at a time. Then of course there are the Inuit, and the Masai. This of course does not prove that LC is the best diet. It does suggest strongly that HF is just fine when combined with animal proteins and the micronutrients which are derived from these. However, when one’s health shows signs of glucose intolerance, would that not suggest that eating more glucose generating foods like fruit and potatoes is not really the best course of action when other alternatives are available which are known to be beneficial? Like I said, you can always change to a different diet if LCHF is not for you. No harm done. Let’s agree to disagree.
“I think that micronutrients and MCFA produced in the gut are not the main issue here. ”
It is SCFAs, to be precise. I do not agree with your opinion.
“I would have thought that hunters and gatherers ate mainly a HFLC diet. ”
Thoughts do not matter, sorry. What matters is evidence. Read my recent comment linked below and note the high fiber intake of ancestral populations. (No way you can reach it on a diet of 60 g of carbs a day or so).
“The findings surprised us,” – high levels of HDL cholesterol may increase a person’s risk of premature death, according to new research. https://www.sciencedaily.com/releases/2016/08/160811190922.htm
Here’s an anecdote about the all-important self-awareness we often seem to lack. I had some thrust upon me on one occasion when I found myself in a traffic queue. It was at a place where I had sat in a queue many times before. I felt, as usual, uptight about it. The difference on this occasion was that I was visiting some people who were not far away and it was far too early for me to arrive. The traffic queue was working in my favour but it summoned up my habitual behaviour.
(And of course, even if I hadn’t been so early, there was nothing I could have done about the traffic, eh?)
Did you then calm down? Heart rate and blood pressure decrease?
To what degree could you then control your body’s system’s responses?
could you slough it off, or was it like meeting the tiger in the bamboo?
What I’m wondering is: Do SOME of us have physiological responses beyond control, beyond the reach of meditation, exercise, mindfulness, etc?
Hello JDPatten
I didn’t need to calm down much as I do not think my reaction was above what most other people’s might have been. I simply gave the example to show how we react out of habit and so not always according to circumstances, and how we reinforce our behaviour. But I think the incident led me to be more relaxed in traffic jams.
Your reactions sound natural and commonplace, if rather strong. Since they are short bursts of HPA activity rather than relentless chronic stress/strain, they should not be allowed to give you the more harmful type of anxiety through worrying about them after the events. Also, any panic about them at the time they occur will only reinforce them (and may have already added strength to them) – quite the opposite of desensitisation! Try to see the episodes as relatively harmless. I hope this helps and doesn’t sound flippant. Perhaps Dr Kendrick or any psychologists watching the blog could give you a more informed opinion. Very best wishes.
Hmm. Diana worries that I don’t get enough fiber, but I think I have eaten a pretty high fiber diet in general. I may not be the right person for a HFLC diet, and yet I suspect that I am not particularly unusual and that I am just the sort of person to benefit. That is, I’ve got all the symptoms of someone who needs to cut back on carbs. But now Diana has revealed that she does not really believe that it is good for anyone. Diana I’m wondering why you think there is no basis in human history of people doing well on such a diet? I can agree that some low carb people go to an extreme, which I am avoiding, but there are people who do not have access to grains or did not I should say, and of course they ate carbs but most likely never got to the point of stressing their bodies like people do today with reams of empty calories which are carbs., no exercise and constant snacking. The total amount of carbs was just not there. Also, the articles you linked are a bit too academic and they didn’t cut to the chase in the conclusion. What was the conclusion? I am very interested in the gut microbiome as a partner in health.
John, as for the need to cut back completely I dunno. That my body can’t reset itself under a regime of 2 meals a day and a 16 hour fast every day and a dinner that includes a carb like potatoes? Is that substantial carbs? Probably in a strict view it is. I might be eating 60 to 100 grams a day. By the way, I’ve been eating relatively low carb and high fat for quite a while. But that’s relative to average Americans. Still probably way too high.
Maybe television, video games and the internet are as responsible for the obesity problem as diet. But there is a definite progression over 3 generations that is sobering.
It’s all relative.
Low carb devotees and advocates generally recommend a maximum of 50 grams per day and an ideal of less than 20 grams.
Anna
“I think I have eaten a pretty high fiber diet in general.”
You think, really? It can be counted. Use a nutritional calculator and see for yourself. You may be surprised.
” Also, the articles you linked are a bit too academic and they didn’t cut to the chase in the conclusion. What was the conclusion?”
Sorry. The paper I linked basically said that if you eat fiber and your gut flora produces the right metabolites (SCFA propionate was mentioned) then your blood pressure is lowered: “indicating that SCFAs produced by the gut microbiota likely influence blood pressure regulation.”
Anna, Gary Taubes, Zoe Harcombe and others are quite clear that exercise has little influence over weight. This is the calories in and calories out model that they believe is wholly discredited. It’s the idea that Coca Cola and the food industry have spent millions to promote. It means if we’re fat, it’s our fault and nothing to do with the junk they produce and we’re encouraged to eat. The Times exposed their tactics earlier this year.
There were almost no gyms in this country in the 1970s and few people were obese. I’ve exercise all my life but my weight has only changed when my diet changed. About fifteen years ago I began to drink fruit juice liberally because it was became freely available at work and I assumed it was a healthy drink. I began to put on weight for the first time in my life. I stopped drinking the fruit juice and my weight returned to its previous level. About two years ago I adopted a low carbohydrate and high fat diet. Without effort or hunger I lost about a stone and returned to the same weight that I was in my twenties. I feel more alert mentally and better physically. I have no idea why, but a slight tremor in my left hand disappeared and a couple of old skin blemishes on my arms went from brown back to normal skin colour. Of course this can all be dismissed as ‘anecdotal’, but it’s the best evidence possible for me. An anecdote is a case study for those with an open mind.
“There were almost no gyms in this country in the 1970s and few people were obese. ”
I agree, and I am old enough to remember the late 50’s onwards. Some people will tell you that we were all fitter back then because we didn’t have so many cars, but in truth, we simply spent a lot of time waiting for and sitting on buses, and after school or work, the lack of a car meant that we went home, rather than visiting a sports centre or whatever.
If I had returned to those times when I retired (that would need some serious technology!) I know I would have taken far less exercise than I do now. You need a car to drive to an off-road bike track (alternatively you can get there on the roads until you get knocked down), and you need good transport (ideally a car) to get to any kind of sports centre. There are more gyms and sports centres now because people can actually get there with reasonable effort.
For years, the Atkins diet was accepted as slimming but supposedly bad for you (all that saturated fat). Some people took that supposed risk in order to get slim efficiently. Now it clearly makes sense to bias your diet in that direction.
However, I suppose I do worry about the more extreme low carb diets – basically because they are extreme diets, and I think the only way we are likely to become short of other nutrients (vitamins etc) in the West, is to eat an extreme diet.
David Bailey
Let me comment anecdotally:
I had two periods of prolonged immobilisation due to operation/injury this year. During this time I had to sit around, ate too much and put on weight. I am gradually now shedding this weight by a combination of not eating so much and exercise. I have read all the authors, Taubes, Harcombe, et alii.
My own anecdotal opinion is that exercise shakes up the gut and somehow improves metabolism.
In one of the Alice books I remember reading about believing two impossible things before lunch. That seems to work also.
World J Gastroenterol. 2012 Sep 7; 18(33): 4593–4596.
Published online 2012 Sep 7. doi: 10.3748/wjg.v18.i33.4593
PMCID: PMC3435786
Stopping or reducing dietary fiber intake reduces constipation and its associated symptoms
Kok-Sun Ho, Charmaine You Mei Tan, Muhd Ashik Mohd Daud, and Francis Seow-Choen
Author information ► Article notes ► Copyright and License information ►
This article has been cited by other articles in PMC.
Go to:
Abstract
AIM: To investigate the effect of reducing dietary fiber on patients with idiopathic constipation.
METHODS: Sixty-three cases of idiopathic constipation presenting between May 2008 and May 2010 were enrolled into the study after colonoscopy excluded an organic cause of the constipation. Patients with previous colon surgery or a medical cause of their constipation were excluded. All patients were given an explanation on the role of fiber in the gastrointestinal tract. They were then asked to go on a no fiber diet for 2 wk. Thereafter, they were asked to reduce the amount of dietary fiber intake to a level that they found acceptable. Dietary fiber intake, symptoms of constipation, difficulty in evacuation of stools, anal bleeding, abdominal bloating or abdominal pain were recorded at 1 and 6 mo.
RESULTS: The median age of the patients (16 male, 47 female) was 47 years (range, 20-80 years). At 6 mo, 41 patients remained on a no fiber diet, 16 on a reduced fiber diet, and 6 resumed their high fiber diet for religious or personal reasons. Patients who stopped or reduced dietary fiber had significant improvement in their symptoms while those who continued on a high fiber diet had no change. Of those who stopped fiber completely, the bowel frequency increased from one motion in 3.75 d (± 1.59 d) to one motion in 1.0 d (± 0.0 d) (P < 0.001); those with reduced fiber intake had increased bowel frequency from a mean of one motion per 4.19 d (± 2.09 d) to one motion per 1.9 d (± 1.21 d) on a reduced fiber diet (P < 0.001); those who remained on a high fiber diet continued to have a mean of one motion per 6.83 d (± 1.03 d) before and after consultation. For no fiber, reduced fiber and high fiber groups, respectively, symptoms of bloating were present in 0%, 31.3% and 100% (P < 0.001) and straining to pass stools occurred in 0%, 43.8% and 100% (P < 0.001).
CONCLUSION: Idiopathic constipation and its associated symptoms can be effectively reduced by stopping or even lowering the intake of dietary fiber.
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3435786/
Mike Cawdrey, you said in a comment of Aug. 31 –
“Persistent hyperglycaemia is what affects me despite 24-36 hours fasting.”
I met a youngish woman once at the tennis courts who was fit and seemingly in good health. However, I discovered from conversation that her glucose levels were in the 11 mmol/l range pretty steadily. He was about 35 years old and following her doctor’s advice which was based on medications. Her doctor believed she was insulin resistant and had her on Metformin among other drugs.
While talking with her, I did not detect any other outward signs of high glucose levels or insulin resistance, such as overweight or lacking in energy. I suggest a low carb diet to her which she tried and when I met her again after a couple of weeks she said that the low carb diet was better for her.
Then some months later, I was re-reading a book called “The World Turned Upside Down: The Second Low-Carbohydrate Revolution” by Dr. Richard David Feinman, a professor of Biochemistry at SUNY, a university in NY, USA. He teaches biochemistry to medical students. There was a chapter on a case concerning Wendy Pogozelski, a Professor and Chairman of Biochemistry also at SUNY.
You should do a search on that name a read some of the stuff there. She developed adult type I diabetes and the doctors did not diagnose it properly. They did not check her insulin levels. In the end she diagnosed herself, but the story is quite interesting in how she did it all.
After reading about this case again, I thought of this youngish woman tennis player. I immediately sent her all the information that I had and suggested to her that her problem may be her pancreas and her insulin levels, which all made sense to me. I later found out that when she confronted her doctor and suggested to have her insulin measured, he refused and said that it was not necessary. She insisted however, and it turned out that she was indeed hypoinsulinaemic and he prescribed insulin injection which helped immensely and set her on a path to glucose control.
You probably know that in a case where you are metabolically defective, and insulin levels are lower than required for Glucagon control (insulin inhibits the production of Glucagon), the body continues to produce glucagon in spite of there being ample levels of glucose in the blood already. It is as if the body doesn’t know that glucose is already abundant because insulin is too low. So if your body has difficulty making enough insulin to control blood glucose, glucagon production will not be shut down properly and your body will continue to make glucose even though you already have an abundance in the circulation. Your blood glucose problem may be due to insufficient insulin levels. You may have the same problem.
You might also want to read this post in a blog by Professor Grant Schofield.
http://profgrant.com/2016/01/29/understanding-glucagon-and-somatostatin-28/
John U
While I am not in my thirties by a very long way, (84th decade) I am marginally overweight (Flegal et al: JAMA. 2013;309(1):71-82. and two previous reports) to quote:
According to the results presented herein, overweight (defined as a BMI of 25-<30) is associated with significantly lower mortality overall relative to the normal weight category
I am therefore happy weight wise. I had come to the conclusion that a low insulin level might well be the cause and I asked my GP to have it tested; he referred it to the Trust “expert” who claimed that “they never did insulin levels because the treatment was the same whatever the level”. I have also had an MI (probably due to stress) which was dealt with by a stent and two “topups” to five stents without any angina or other cardiac event.
May I thank you very much for your advice it will prove most useful.
While I am not a doctor, only a vet, but with nearly six decades of research experience (including nutrition, drug trials etc plus expert reports for drug authorization) and several patient reviews of studies for the BMJ, a journal with a very novel and forward looking policy of involving patients in the system.
One observation that I came across regarding diabetes and heart attacks was that the addition of insulin therapy post-MI substantially increased increased the risk of dying, presumably due to excessively raised insulin levels. Without knowing ones insulin levels one is somewhat cautious of asking for such treatment. Your comments are therefore of great value to me and possibly others as well. Unfortunately I cannot reveal the source of my information.
Thank you to for the link. Most interesting
Read “84th year ” NOT 84th decade. A right crazy slip there
Mike,
I hadn’t realised that you are in your “84th decade” – you are doing extraordinarily well for that age! You must be one of very few people to have witnessed the birth of the printing press, and Windows 10!
John,
Thank you for this “reminder”.
“You probably know that in a case where you are metabolically defective, and insulin levels are lower than required for Glucagon control (insulin inhibits the production of Glucagon), the body continues to produce glucagon in spite of there being ample levels of glucose in the blood already. It is as if the body doesn’t know that glucose is already abundant because insulin is too low. So if your body has difficulty making enough insulin to control blood glucose, glucagon production will not be shut down properly and your body will continue to make glucose even though you already have an abundance in the circulation. Your blood glucose problem may be due to insufficient insulin levels. You may have the same problem.”
This reminded me of one of the most informed “scientific” Prize Lecture I ever came across, by Professor Robert Unger, on this subject and a lecture that cannot be listen to too many times in my opinion. The lecture is turning many of the established views on diabetics upside down. E.g. the glucagon producing alfa-cells have turned insulin resistant and in addition the beta-cells have turned “sick” and are not able to produce the insulin spikes, necessary to turn the beta-calls off, as healthy cells do when blood glucose suddenly rise. It is, according to Professor Unger, not by coincidence that alfa- and beta-cells have evolved in intimate contact with one another – it is the “insulin chock” spike that turns the glucagone production off.
FYI – Media watch – it’s all in the Sun! (a UK newspaper)
It’s been CVD week in the Sun, and elsewhere I guess, and by coincidence seems to tie in with some of the topics under discussion in this current blog by Dr K:
Here are the headings…
From Mon 29 Aug:
“Eating like the Med better than statins”
From Tues 30 Aug:
“10 min docs a risk to patients”
“Women heart fails ‘missed'”
From Thurs 1 Sept:
“After 7pm scoff will see you off”
“Families fury as NHS exec gets new £240K job”
Regards!
J Geriatr Cardiol. 2015 Jul;12(4):439-47. doi: 10.11909/j.issn.1671-5411.2015.04.017.
Significant roles of anti-aging protein klotho and fibroblast growth factor23 in cardiovascular disease.
Ding HY1, Ma HX1.
Author information
Abstract
The klotho gene has been identified as an aging suppressor that encodes a protein involved in cardiovascular disease (CVD). The inactivation of the klotho gene causes serious systemic disorders resembling human aging, such as atherosclerosis, diffuse vascular calcification and shortened life span. Klotho has been demonstrated to ameliorate vascular endothelial dysfunction and delay vascular calcification. Furthermore, klotho gene polymorphisms in the human are associated with various cardiovascular events. Recent experiments show that klotho may reduce transient receptor potential canonical6 (TRPC6) channels, resulting in protecting the heart from hypertrophy and systolic dysfunction. Fibroblast growth factor23 (FGF23) is a bone-derived hormone that plays an important role in the regulation of phosphate and vitamin D metabolism. FGF23 accelerates urinary phosphate excretion and suppresses 1,25-dihydroxy vitaminD3 (1,25(OH)2D3) synthesis in the presence of FGF receptor1 (FGFR1) and its co-receptor klotho, principally in the kidney. The hormonal affects of circulating klotho protein and FGF23 on vascular and heart have contributed to an understanding of their roles in the pathophysiology of arterial stiffness and left ventricular hypertrophy. Klotho and FGF23 appear to play a critical role in the pathogenesis of vascular disease, and may represent a novel potential therapeutic strategy for clinical intervention.
KEYWORDS:
Cardiac hypertrophy; Cardiovascular; Fibroblast growth factor23; Gene polymorphisms; Klotho; Vascular calcification
PMID: 26347327 PMCID: PMC4554784 DOI: 10.11909/j.issn.1671-5411.2015.04.017
Continue with Klotho
Researchers recently found that a single gene may account for as much as 3% of total variation in human intelligence. If this result holds, it suggests some obvious strategies for developing new kinds of cognitive enhancers since it implies that a single protein (klotho) may be responsible for as much as a 6 point IQ boost.
To put this in perspective, there were previously no other single-point genes believed to account for even a 1 point IQ gain. And a 6 point IQ boost is almost the difference between the average farm laborer and the average elementary school teacher. So this could be a big deal.
And the longevity benefit of klotho is even more well studied and potentially larger than the cognitive benefit. For example, when researchers checked to see how common the KL-VS gene is at different ages, they found that by age 79+, there’s a 1.57x odds ratio in favor of having this gene despite there being a 4x odds ratio against having it at birth. Klotho gets this effect by being extremely cardio-protective via a unique pathway that helps regulate blood calcium levels much better as folks age.
So how can you benefit from this? For one, you can check 23andMe right now and look up if you have a functional copy of KL-VS. Either click the link to 23andMe or check your raw data file: look for Rs9536314 and if it’s GT, you’re already one of the lucky folks (1 in 5) with high klotho levels and potentially boosted longevity/cognition.
But what if you’re TT or GG? That’s where it gets interesting. All the articles recently published about klotho are repeating boilerplate from the researchers about how “someday maybe someone will find a drug to boost klotho levels”. Well, since Google Scholar and Library Genesis exist, that day is today and that researcher is me.
It turns out that lots of people get their klotho levels increased as a side-effect of taking prescription forms of “activated” vitamin D (VDRAs) for chronic kidney disease (CKD). But there’s no reason to wait until you’re almost dying and need dialysis to start benefiting from this knowledge. Instead, this implies that taking something like 0.25 mcg/day of Calcitriol or 1 mcg/day of Paricalcitol right now for someone without the beneficial KL-VS variant of the KL gene might actually give a huge longevity and IQ boost. The intelligence boost is so large, that if this new study is right and the effects of klotho are at all acute, you should be able to measure it directly with something like quantified mind or perhaps even just raw introspection. Hopefully lots of researchers follows up on the most obvious implications of these two currently unconnected research findings and investigate activated vitamin D as a way to boost longevity and cognition in the 80% of the population lacking functional, klotho producing KL-VS genes.
Mendelian randomization study finds no relationship between vitamin D status and coronary artery disease
Posted on August 17, 2016 by Amber Tovey
A recent Mendelian randomization study published in the journal Circulation: Cardiovascular Genetics found that genetically low vitamin D levels were not associated with increased risk of coronary artery disease (CAD).
CAD, also known as heart disease, is the leading cause of death in the United States. It occurs when cholesterol-containing deposits, called plaques, begin to develop in the coronary arteries. The plaque buildup narrows the coronary arteries, which reduces blood flow to the heart. As a result, chest pain, shortness of breath, irregular heartbeat and light-headedness are common symptoms. In some cases, the artery can become completely blocked, causing a heart attack.
Observational studies have suggested that low vitamin D levels are associated with an increased risk of CAD-related events. Therefore, researchers have become interested in whether vitamin D supplementation may play a role in the prevention of mortality and morbidity due to CAD.
Researchers recently sought to find this out by conducting a Mendelian randomization study.
Mendelian randomization studies possess the ability to prove causation, similar to a randomized controlled trial (RCT). Instead of randomly dividing study participants into two groups, the control and experimental groups, Mendelian randomization utilizes nature’s randomization of genes. In this study, the researchers assessed the genotypes of 22,233 individuals with CAD and 64,762 individuals without CAD, searching for individuals who have genetic variants that are associated with low levels of vitamin D. The researchers found that individuals who were genetically predisposed to low vitamin D levels had the same risk for developing CAD as those who were not predisposed (OR 0.99, p = 0.93).
The researchers summarized their findings,
“…Our study provides evidence against a causal role for vitamin D in CAD susceptibility.”
They went on to state,
“These findings suggest that previous observational epidemiologic associations may have been influenced by confounding or reverse causation.”
While these findings conflict with observational studies, they are consistent with a previous Mendelian randomization study’s results. The previous study determined that low vitamin D levels were related to increased all-cause mortality and cancer mortality, but not cardiovascular mortality.
The recent study possessed several strengths worth recognizing. As mentioned earlier, a Mendelian randomization study has the ability to prove causation, making it one of the strongest study designs. Furthermore, the study used a large population sample. Lastly, the study’s results represent the relationship of a life-long exposure to reduced vitamin D levels. Since vitamin D is unable to be patented as many medications are, long-term RCTs on the effects of vitamin D on CAD are unavailable.
Citation
Tovey, A & Cannell, JJ. Mendelian randomization study finds no relationship between vitamin D status and coronary artery disease. The Vitamin D Council Blog & Newsletter, 2016.
Source
Manousaki, D. et al. Mendelian Randomization Studies do not Support a Role for Vitamin D in Coronary Artery Disease. Circulation: Cardiovascular Genetics, 2016
Errett
Now that is one tough paper to read – lots of acronyms etc. They cite several RCTs but if one actually looks at individual studies many are comparing VitD RDIs(400-600 IUs) with placebo. One trick Big Pharma uses when comparing treatments is to use minimum doses of the “competitor” product. An example of this is in the 2×2 factorial HPS study. The second treatment was an anti-oxidant vitamin cocktail including Vit E but EXCLUDING CoQ10 (an established anti-oxidant) for which Merck has a patent combining CoQ10 with simvastatin, the second treatment in this study. I would also point out that the AMA has been trying to turn vitamins into POM drugs for years. Prof Gotzsche’s book is well worth reading as is Dr Kendrick’s “Doctoring Data”
Mike,
What you say is in accordance with what I have “learnt” during my 17 CVD-years now.
E.g., having done my proper “homework” (Linus Pauling, Shute e.g.) I now keep my unstable angina reasonably in control since two years now with 1600 IU natural vitamin E daily. When you dig into this and find studies telling you that it is “useless” it seems that without exception they are using not only very much smaller doses without therapeutic value but also the synthetic variant of E-vitamin which also seems to be without value. Behind such papers a Big Pharma “agenda” is to be suspected, not least by me.
Mendelian Randomisation = big can of worms
And then there is this
https://www.sahmri.com/our-research/themes/heart-health/theme/theme-highlights/auspice-%E2%80%93-can-cardiovascular-event-risk-be-reduced-following-pneumococcal-vaccination
Six ‘acronyms etc’ in nine lines, Mike. Tough reading indeed.
I read ‘Why Zebras don’t get ulcers’ many years ago, and it is one of the books that changed my life. Because I started as theoretical physicist I too did not like the stress – stress. I never wanted to use the word ‘strain’ for hormonal response because ‘elastic strain’ is near hard wired in, but I will see it like operator overloading in programming languages.
The argument about men in Latvia & Lithuania is a good one, but there may have been disruption in food in 1989 so food could still be part of the reason – let’s say in the stable communities before 1989 the rural people had the ‘right’ nutritional mix, but after 1989 a lot of black markets sales started so that the good food was shipped out. This would be like the current fashion for quinoa where South Americans are selling it and eating other grains that don’t have the range of essential amino acids that quinoa has.
I will work through the comments now as this XX seems to have stimulated many.
I haven’t read Sapolsky’s “Why Zebras Don’t Get Ulcers”, but I used to love watching the herds of zebra grazing peaceably in Etosha Pan game reserve in Namibia, and wondering to myself what they were thinking. I came up with two answers:
— “Mmmmm. Grass! I love grass. I could eat it all day. And if I finish this clump of grass, why worry, there’s another clump of grass. In fact, there’s grass all the way to the horizon. I’m in grass paradise. I’m so lucky. God has been good to me.”
— “Bleccch! Grass. I hate the stuff. But it’s all there is. And if it isn’t brown and tough, or someone’s pooped or peed on it, it’s been trampled it into the dirt. It’s the same all the way to the horizon. I’m in some sort of grassy hell. What have I done that God has punished me?”
Mendelian randomization approaches have the potential to contribute to an improved understanding of the aetiological importance of environmental factors in common chronic diseases, through reducing the influence on estimated associations of confounding, reverse causation, and various other sources of bias. Categories of inference from Mendelian randomization studies involve propensity to being exposed to a risk factor, proxies for intermediate phenotypes, modifiers of environmental exposures, studying intergenerational exposures, and identifying the broad categories of exposure that may be aetiologically important, and thus should be investigated further. Limitations of the approach must be acknowledged; most are common to any genetic epidemiology enterprise and some should be reduced through application of the growing knowledge provided by the study of functional genomics.
http://ije.oxfordjournals.org/content/33/1/30.full#T4
From Ivor—-very interesting piece—-suggesting stress may be tied to CVD
http://www.thefatemperor.com/blog/2016/9/4/cac-calcium-the-ultimate-test-for-atherosclerosischallenges-ldl-as-cause
About supplement studies – you can find studies that supplements are “no good for you” but if you dig deep you will find alot of big pharma paid people and or the researchers use the wrong supplement and or the dose is inadequate.
Oh, dear, I made along post with replies to people, pressed the button and ended up in June. At the risk of double posting, I guess I’ll post it again.
I feel the need to talk about diet because I am convinced it is very important to this issue and other health issues. I also find it puzzling that CVD could be going down when 50% of the kids I see are fat, and 75% of 30 year olds. My daughter who lives in Sweden tells me there are very few fat people, and the way they eat is VERY different. Now, someone mentioned exercise does not help you lose weight. Well, first of all I do not think that is true if you exercise on a regular basis. It does slowly change you. And the few people I know who are truly physically active are lean, irrespective of age. But exercise is not necessarily about weight loss. It’s about having good health, oxygenation and less insulin resistance, lower blood pressure and cardiovascular fitness, etc.
Diana, thank you for the explanation. While I think that I need to be HCLF, I am still a bit puzzled as I feel this whole situation is multifactorial and that something has gone wrong when people have to limit carbs to such a degree. As to using a nutrition counter, the only thing I have ever been willing to put in some real effort to counting is carb grams, so that I can get a good feel for it. I know what foods contain fiber.
Stephen T, I am not into calories in-out. Check out some Jason Fung videos about that. He’s a kidney doctor who treats many diabetics and got really serious about understanding insulin resistance and reversing it with diet and fasting. What’s a stone? About 20 pounds? As for your health reversals, I would like to present an article on this whole subject, one reason I found it interesting is the large number of interrelated health issues that go wrong when one has high levels of insulin.
There were a few things he said near the end about what type of fat to eat that I suspect are wrong, but this is a very interesting speech indeed, making the case that yes, it IS all about insulin! It is called Insulin and its metabolic effects.
http://articles.mercola.com/sites/articles/archive/2001/07/14/insulin-part-one.aspx
The low fat craze got to the point that I several times found articles about diet and health and our paleo ancestors as well as Native Americans which stated that they ate lean meat! Hah!! that is absurd. Humans love the taste of fat and most certainly were not throwing away that fuel!
A stone is 14lb.
If carbs have to be severely limited, something is wrong, as you know. But it seems it is very common for it (insulin resistance) to be wrong.
Mark Sisson has some interesting thoughts on how exercise can aid weight loss (I get the feeling you might already know this), and he isn’t a CICO believer either.
Anna, some of the health improvements from low-carb are a mystery to me, but I’ll happily take them! I’ve exercised all my life and think it is good for us in many ways, but marginal when it comes to weight loss. The problem for me is that people are continually told to exercise to lose weight and it’s going to fail for most people. Overwhelmingly it’s about what we eat – the sugar and flour you refer to. When you look at how much exercise is needed to lose a small amount of calories, then it’s bound to fail. I think it’s an hour’s exercise to lose a Mars bar. I swim for thirty minutes, so that’s half a Mars bar. Insignificant. I see people leave a gym and have a muffin and fruit juice. That’s far more calories than they’ve used. Thank you for the reference to Jason Fung. I’m aware of his work and the fasting part is interesting and makes sense to me.
I’d repeat my point that I’ve exercised all my life and my weight has only varied when I’ve changed my diet. I now weigh the same as in my twenties and rarely eat three meals a day. The higher fat content in my diet satisfies my appetite, whereas carbs increased it. As Dr Mark Porter commented in his Times column, I wish I’d known about this years ago instead of following the low-fat nonsense.
Re Exercise
Following my heart attack 4 1/2 yrs ago, until about a year ago, I was physically very inactive (in part due to arterioschlerosis in the legs). But then I discovered a (free!) NHS gym course that nobody told me about, that lasted 12 weeks and a discounted membership to gyms in Lambeth.
At the beginning of the classes, even though I had and have a pretty healthy diet, I had put on around 7 kilos (I’m small-boned and ever since my teenage years, I’ve not weighed more than 60-62 kilos, around 140lbs). After a year of pretty constant exercise (nothing dramatic, at most a selection of workouts for my heart and legs, around 45mins-1hr, three-five days a week), I’ve lost that extra 7 kilos and I’m back to my teenage weight!!! I’m 71.
On top of that, I’ve tried to cut out most of the sugar I consumed (though I use a little honey and unrefined sugar, half a teaspoon in my tea and coffee), and I’ve never consumed ‘soft drinks’, fast food or pre-prepared meals. Smoking was my one big mistake and I’m pretty sure it’s the major cause of my busted body.
So, exercise by itself doesn’t work, nor does diet, again by itself. Surely it’s a holistic approach to taking care of one’s body that delivers the goods?
Had you stopped smoking before your event?
Bob: Yes, I stopped smoking almost 7 years ago, around three before my ‘event’, but of course, the damage had already been done. BTW, once I decided to stop, I just did, no patches, hypnosis et al, and no withdrawal, I just stopped.
@ Stephen T
Unfortunately most people’s idea of exercise is half an hour of moderate jogging or leisurely swimming. This is trivial, non-existent calorie burning compared to the work we used to in 6 days of manual work or earlier still, in hunting for our food.
Fortunately there is a trick: High Intensity exercise which changes your metabolism. Half an hour of moderate exercise, as you say burns half a Mars bar. 20 secs of severe high intensity exercise makes your muscles hungrier so that they are still burning calories when you return to your desk or have your feet up watching television. So 20 secs of high intensity exercise produces 24 hours of calorie burning!
My thrice weekly bike ride involves a 200yd hill which I attack absolutely flat out. Afterwards it takes at least a minute before I can breathe comfortably again. That 200yd hill I believe does more good than the other 10 miles of the route.
MalcolmS
I am 77 and can buzz along on the converted railway line cycle paths, largely flat with not that much effort, according to my heart rate monitor, but on the way ho, come the hills, and it is a different story.
I think they do me good, they certainly get the heart beating.
@MalcomS: and doesn’t it feel good to get the “ticker” going at high speed?
That’s because those fat kids haven’t yet developed CVD and a host of other health issues. Give it a few decades and they will (provided they stay fat, of course).
Diana,
You cited an article about paleolithic diets that I intended to respond to but now can’t find. Perhaps it was a commentary from my detour into June? I just wanted to say that while it is very true, humans being omnivores, that those different peoples from 10+ thousand years ago ate a lot of fiber and some 250 or more different plant species, I am not sure it is useful to compare that to the way that people eat now, lots of sugar, lots of flour, lots of white flour even if they also eat whole grains, and a few vegetables. This is one reason I have taken on a hobby of expanding my foraging abilities and the eating of wild foods. There are many edibles where I live. One goal I have it to make something palatable with acorn flour.
Anna, what do you forage?
It seems that many of us commenters here are still interested in food at the expense of considering the subject of this blog entry. We are at XX.
It seems you need a heavier hammer to nail your points, Dr Kendrick.
JDPattern
Agree!
I feel guilty 🙂
I just had a fight with the waiter in the luxury restaurant in lappish wilderness in Kautokein0, Norway, about avoiding sweet desserts – all were sweet on the menu but we managed after sincere negotiations to get a plate with assorted cheese. My strong argument was our severe health condition so they made their best in the kitchen.
Excellent, Goran. You can only get results by challenging the status quo.
But, what harm did you do to yourself with the “fight” and the “strong argument”??
Jd
If you do a rough analysis of the comments on this blog series, they fall roughly under the following headings
Diet
Supplements and arcane observations, on an inverted pyramid basis, i.e much theory based on little fact,
Our dear Dr K, points us towards what are now called “life style factors” but very little comment on that.
Why?
I completely agree! One of the things that many posters ignore, is that the crazy demonization of saturated fat and cholesterol, tells us that medical science in this area is BROKEN! There really isn’t another layer of reliable science waiting to be uncovered, wehave to go back to common sense.
Some people are keen on the most obscure wonder-supplements, but medical scientists seem very ready to believe things that aren’t even approximately true – think of the HRT treatments that were thought to help with CVD, and actually caused it (plus some cancer). That was only revealed when an RCT was performed.
How many obscure supplements have been tested in an RCT – approximately none, I would guess – so you can’t even be sure these things aren’t doing harm!
The problem with lifestyle factors is, how do you enumerate and quantify them?
At least with diet you can name and weigh from coarse to fine detail e.g. X grams of fats, Y mg of vitamin C etc.
Smoking is measurable, but what about second-hand smoke and polluted air?
Take stress. Worry, anxiety, fear, responsibility, etc, all contribute to stress, but are they all CVD-relevant, and how do you quantify them? Some people can live on $5 a day, others would be terrified if their income was cut to $50 a day.
Or exercise. What constitutes moderate exercise, given that we are all physically different? And what type of exercise are we talking about — flexibility, strength, cardio etc?
Congratulations you have made the case completel for statins and against your own site all in a few paragraphs. Let me explain. If I am given statins – and sites such as this disappear – and I BELIEVE statins will work then I will be less stressed and therefore CVD risk falls. In addition statins DO lower cholesterol (you agree). I see the figures and my belief is cemented and stress further reduced. If at the same time I go on low carb and either low fat or high fat – as long as it is low carb then my diabetes risk falls, fasting blood glucose figures improve and these ALSO give me confidence and reduce stress and thus reduced risk of CVD. If I also do some exercise to help me unwind, socialise but drink water, further unwinding then stress further falls.
So – more statins, more sleep, low carb diets, restriction on information that might make me lose belief – and that’s CVD sorted!
Ah – I lived in that blissful state for a while (3 years) – thinking of my Simvastatin tablets as ‘live longer pills’. Then the side effects struck, and the stress of that was very considerable!
George McWhirter:
Eh? You have established zero connection between your stress and people discussing statins, let alone that stress CAUSES heart disease. And the fact that statins lower cholesterol (true) does not prove that cholesterol CAUSES heart disease. In fact you can argue that excess cholesterol is merely a symptom of heart disease but not the cause. Even my consultant fellow agreed that cholesterol is part of the package of defensive mechanisms the body produces in order to REPAIR damaged arteries.
This whole blog entry is about stress/strain and heart disease. Quote: “Data that links the work of Sapolsky and Bjorntorp who, in my opinion, ought to be recognised as the man who established, beyond doubt, how negative stressors can create measurable dysfunction of the HPA-axis which leads, in turn, to the metabolic problems that cause CHD. Or, to put it more simply. How stress causes heart disease”
My point about statins and cholesterol was that if you BELIEVE cholesterol causes heart disease and statins lower it then you will BELIEVE your CVD risk is less which will reduce your worry…which will reduce CVD. Self-fullfiling prophecy.
Therefore if the GP gives you a placebo but you BELIEVE it will reduce your chances of CVD THEN it will because of the reduction in stress that this belief will cause. Therefore any information that says otherwise and deals with other causes may, ironically, cause disquiet and thus increasing the chances of heart disease.
Data, data please. If what you say is true then there should be data on the treatment of heart disease with placebos that actually works. Moreover, nobody is denying that stress could be a part of the problem but as others have said here, how do you measure it (aside from adrenaline but this is a flight/fright response)? And anyway, is a cause or yet another symptom? Surely, as Dr Kendricks has stated here, when we talk about heart disease, the first thing to be mentioned is smoking (I assume this part of the ‘lifestyle’ assessment). I’m pretty sure smoking was the most significant cause of my heart attack.
BTW, if I remember correctly, nicotine is one of the strongest anti anxiety drugs known to us. Which doesn’t stop cigarettes from quite possibly increasing incidence of CVD. While making us calm in the process.
Where’s the data to suggest that smoking relaxes anyone other than addicted smokers? They do it because they’re addicted, not because it’s just like yoga.
Google “psychoactive effects of nicotine” and it will give you all the data you need. Saying that “smokers smoke because they are addicted” doesn’t make sense. It’s actually a fine example of circular reasoning, if I am not mistaken.
I think we should then do everything possible to keep our “disquiet” at bay. Let’s not talk about CoQ10 depletion, liver damage, cognitive decline, or neuropathies that can and do come with statins. With BP meds we shouldn’t think about ortho static hypotension and weakening of the heart. With aspirin let’s not mention gastrointestinal bleeding.
Let’s just pop pills without asking questions since asking questions can increase disquiet! In fact, maybe we should apply this attitude to all other areas of our lives. Who needs to think, thinking can be so disconcerting.
I’d rather than have aspirin than many other anticoagulants.
HBP is supposed to be the major cause of strokes etc etc. yet these people have high blood pressure and live for ages: http://www.independent.co.uk/news/science/italy-acciaroli-scientists-investigate-why-residents-one-town-italy-live-long-a6961371.html
@George McWhirter – “If I BELIEVE statins will work then I will be less stressed and therefore CVD risk falls”
After several attempts at the golf club trying to raise an interest in DrK’s books/blog, I finally got one male golfer to read the blog and give up statins. On his next consultation, his doctor admitted that standard statins did indeed cause muscle aches but that he could prescribe a more expensive brand that had no such problems. So my golfing colleague was straight back on the statins, very happy with the cycle he’d been through, namely that by quitting cheap statins he had gained access to a much better brand of pharmacy. Doh!
On another occasion, I got talking to a female golfer who had previously had very high cholesterol readings (in a women a marker for high longevity) and had been terrified by her doctor that she was in imminent danger of death. She had started taking statins, got her cholesterol levels down and obviously then felt in control of a bad situation. Even though she had severe muscle aches she believed these demons were the price that had to paid for her continued survival. In her case I decided not to even broach the subject of Dr K’s blog in case I robbed her of this sense of control. I reasoned that her doctor induced terror of high cholesterol was probably the greatest danger to her health. Ultimately though, do you really serve anybody’s interest by lessening their trust in their doctor?
My own mistrust is unfortunately now complete and I dread the weigh-scales, BP measurement and severe ticking off for having an alcohol intake of 40 units (three times the current limit of 14 units!!) which makes up the first half of every visit to the quack. I’ve nearly bitten through my tongue by the time I get to talk about the actual reason for my visit!
So presumably you disagree with: https://www.drinkaware.co.uk/alcohol-facts/health-effects-of-alcohol/diseases/alcohol-and-cancer/
You know they got their guidelines from a christmas cracker, of course?
Your comments reveal a very disturbing relationship between us and the medical BUSINESS.
For example, after my heart attack, my BP was measured and it appeared to be very high so I was put on Ramipril (5mg daily). Much later I discovered I was one of those people who react badly to having my BP measured (the white coat syndrome). After a 24hr BP test, it seems I don’t have high BP after all (it’s currently 128/81, not bad really considering), yet my GP wants me to continue taking the Ramipril.
I’m caught in a loop, reliant on the alleged expertise, which if you buck it, all hell breaks loose! A year of tests and cajoling followed my decision to stop the statins (6 visits to hospitals, treadmills, ultrasound, blah-blah-blah), all costing a fortune no doubt and essentially to no real purpose. In fact, as my GP admitted to me, my STRESS was directly the result of my being “over-diagnosed”, and for which she actually apologised (poor thing)! Furthermore, when I said to her,”With all due respect, you’re basically a dealer for the drug industry”, she agreed!
At my final (hopefully) consultant visit last week I told the guy that I’d stopped the Omeprazole/aspirin combo and once the stuff was out of my system I was switching to Lycopene. He flat out said “It doesn’t work” but could offer no proof/sources for his opinion. But he did agree (kindof) that cholesterol was part of the body’s healing process.
So, I figure stress is very much a part, not of my ‘lifestyle’ but directly the result of the medical business injecting fear into my life!
@barbrovsky: do have info on Lycopene?
Re Lycopene: Yes, I tried it for a couple of weeks and gave it up. 1. it’s expensive and 2. you need to take an awful lot of the stuff (the manufacturer recommends 3 of these pills a day, I couldn’t tolerate 1), which is why it’s expensive. 3. I didn’t feel well after taking it and I’m really not sure it does anything at all. It has an immediate effect of making your skin feel like it’s burning and the more you take, the more extreme the feeling is.
I used Fruitflow as a replacement for Aspirin and it claims that it doesn’t contain lycopene but is derived from tomatoes like lycopene https://www.fruitflowplus.com/ufaqs/how-is-fruitflow-different-to-lycopene/
Their site makes claims about bp, circulation etc.
Re Fruitflow: I guess you have stopped taking it. Why? I’m taking fishoil as aspirine replacement.
Eugène: Initially I was trying to find a replacement for the Omeprazole (which is meant to reduce the acid from the aspirin) as that stuff is poison! I came across lycopene/fruitflow and decided to try it out. Gave up on all of it and went back, not to Omeprazole, but to Ranitidine and aspirin which seems to be okay so far.
@George McWhirter – “So presumably you disagree with drinkaware.co.uk: health-effects-of-alcohol ”
Yes. It isn’t easy to get at the real facts on alcohol. On trying to quantify the J-curve, which portrays the BENEFITS of moderate drinking, I spent hours on Google trying to find proper data, namely a graph with real numbers on both axes that wasn’t hidden behind a pay-wall. Eventually I came across the meta-analysis by Giovanni Corrao from 2000/4. The graph is a third the way down this document:
http://pubs.niaaa.nih.gov/publications/arh27-1/39-51.htm
Basically someone drinking 80g alcohol a day (=70 units per week, since 1 unit=8g alcohol) has the same CVD health as a teetotaller. The optimum health occurs at 20g per day (=17.5 units per week). So if you’re drinking at the current limit of 14 units per week you need to INCREASE your drinking slightly to improve your CVD health. Not quite what the doctor ordered is it?
Actually I no longer believe in risk factor graphs such as this. As I repeat ad nauseam, I’m convinced by Grossarth-Maticek’s experiment in which he dispelled 4 out of every 5 CVD death through a purely psychological intervention, thereby proving: stress causes heart disease. It’s just that, statistically speaking, moderate drinkers have a better attitude to life so their improved health derives entirely from the lower stress levels that this attitude confers.
No doubt there are alcohol consumption levels which are dangerous in themselves but the graph proves that they must be well above 70 units per week and as I’m only a 40/week man, I couldn’t give a monkey’s about my doctor’s opinion on the subject.
MalcolmS
You could try this book, recommended on a blog comment earlier
The Good News About Booze (Anglais) Broché – 25 novembre 2013
By Edwards
Here is an excellent book about the benefits and problems of alcohol (it only covers the ethyl variety!):
The style resembles that of Dr Kendrick himself – it is fairly casual, but actually dissects the actual evidence. There is a different J curve for various illnesses, but it would seem that you are only best off with no alcohol if you are liable to become alcoholic.
barbrovsky
Your comments reveal a very disturbing relationship between us and the medical BUSINESS.
Indeed and why would they not be? GSK study 329 and its manipulation (http://study329.org/wp-content/uploads/2015/09/Study-329-Final.pdf; Polderman and a flawed guideline resulting in 800,000 deaths in Europe with the relevant paper retracted (Bouri S, et al. Heart 2014;100:456–464. doi:10.1136/heartjnl-2013-304262; this is the study that on which Cole and Francis based their retracted report).
How many other guidelines flawed?.
And the BMJ 2016;353:i2139 doi: 10.1136/bmj.i2139 (Published 3 May 2016)
Medical error—the third leading cause of death in the US
leading to 250,000 deaths a year (pro rata 50,000 p.a. in the UK) and what is the medical establishment doing about it other than muzzling whistleblowers?
BMJ 2016;353:i2139 doi: 10.1136/bmj.i2139
Also Starbridge B JAMA, July 26, 2000—Vol 284, No. 4
http://www.ncbi.nlm.nih.gov/pubmed/?term=JAMA+2000+284%2C+4+483
US estimates8-10 of the combined effect of errors and adverse effects that occur because of iatrogenic damage
not associated with recognizable error include:
• 12000 deaths/year from unnecessary surgery
• 7000 deaths/year from medication errors in hospitals
• 20000 deaths/year from other errors in hospitals
• 80000 deaths/year from nosocomial infections in
hospitals
• 106000 deaths/year from nonerror, adverse effects of medications (i.e properly prescribed, properly used drugs) . Could this be decribed as “ Death by Guideeline”?
These total to 225000 deaths per year from iatrogenic causes.
And there are other reports that suggest these numbers are an underestimate
and Null, G. et al Journal of Orthomolecular Medicine Vol. 20, No. 1, 2005 21-34
All these references are based on reports in esteemed general and specialist medical journals and govternment reports
The Cholesterol Myth “lower the better”
Mean total cholesterol, men(mg/dl), 2005. Source: BHF-HEARTSTATS
Estimated lowest mortality rates for TC blood levels
All Cause mortality 222 mg/dl 5.75 mmol/L
Non-communicable disease 210 mg/dl 5.49 mmol/L
Cardiac Disease 208 mg/dl 5.44 mmol/L
http://www.heartstats.org/documents/download.asp?nodeib=6797 This URL no longer exists? WHY?
Now on https://renegadewellness.files.wordpress.com/2011/02/cholesterol-mortality-chart.pdf
http://healthcorrelator.blogspot.co.uk/2009/12/total-cholesterol-and-cardiovascular.html
The Congestive Heart Failure Epidemic
The NHBLI/CDC “ congestive heart failure” epidemic Fact Sheet removed from their website but now only on:
https://wayback.archive-it.org/3635/20130901052131/http://library.thinkquest.org/27533/facts.html
The epidemic is rising in lock step with use oof cholesterol lowering drugs. Not what Big Pharma wants and the revolving door system between US govt. agencies and Big Pharma is well known.
QOF
And then there is QOF (Quality of Outcome Framework). This is clearly designed to establish some politically important factors and control of GPs to ensure guideline use.
Is it patient friendly? NO. For example there is no section for reporting patient adverse reactions to drugs. Obviously political issues outrank patient care. In the light of the reports of “Medical Error…” above this demonstrates an element of deliberate cover up!
Do you really wonder at the “disturbing relationship”?
It’s not just the medical BUSINESS, it’s our entire society, from ‘sport’ (another BUSINESS), to ‘education’ (another BUSINESS). Even our legal system has been subverted by big business. Capitalism in the raw, with no controls by the state whatsoever. Our ‘democracy’ has been recaptured by the capitalist class. The bottom line is money, power, control. A digitised, Victorian gangster capitalism, complete with all the trappings of a free society but controlled by an unholy alliance of the state, big business and the corporate/state media.
My GP, who I quoted, is a decent person. She cares but… taking statins is a political/economic decision on the part of the state, she CANNOT speak out against it. Everything is measured against BIG BUSINESS’ bottom line. My GP knows that the giant corps that now dominate society answer only to their shareholders, who for the most part aren’t even people! They’re not interested my health. They’re institutions, many of them far removed from life in this here septic isle.
Privatising the NHS is more than simply making it into a business, it’s an ideological battle to remove the idea of a publicly owned (if not controlled) anything, whether it’s our health, our homes or our schools.
The NHS was perhaps the only decent (and we thought permanent) thing this society has ever accomplished and it wasn’t handed to us, our parents and grandparents fought for it! So if we want to save it, we are going to have fight all over again!
Hello Mike,
in your list of disturbing relationships, you leave out one, corruption. How do you like this, the head honcho of the FDA on a racketeering charge?
Former FDA Commissioner Charged in RICO Lawsuit
A Federal Lawsuit charges Dr. Margaret Hamburg, former Commissioner of the Food and Drug Administration (FDA) with conspiracy, racketeering & colluding to conceal deadly drug dangers – under the federal Racketeer Influenced and Corrupt Organizations law (RICO) law. The amended RICO lawsuit was filed on April 11, 2016 in the U.S. District Court in Washington DC on behalf of eight plaintiffs who claim they have suffered severe harm by ingesting the drug, Levaquin whose deadly risks were concealed to protect financial interests.
The drug is one of the controversial group of antibiotics, including Levaquin, Cipro, Avelox and other fluoroquinolones. Public Citizen petitioned the FDA in 1996 and again in 2006, to issue Black Box warnings for tendon rupture and tendinitis.
?????
yes, you read correctly, the ex-head of the FDA on a racketeering charge.
Mr Chris,
Indeed but I was trying to stick to simple medicine. Corruption deserves a book for itself. Gotzsche has provided an excellent review iin his book (loc cit)
C’mon. Where’s the laughing emoticon ?
(You can’t laugh with your tongue in your cheek.)
I recall Dr Kendricks comment on alcohol consumption “Nothing Stronger Than Whisky”!
Ray
My above comment about tongue-in-cheek was for George’s “Congratulations you have made the case complete . . .”
How could he possibly be serious? Really??
(The “Reply” format here leaves a few things to be desired. A direct reply can get totally lost. After a couple of layers of replies you can’t reply directly at all any more.)
You ask how I can be serious. OK I will talk you through.
1. Do you agree that stress is a major cause of heart disease?
2. Do you agree that there are different types of stress – internal, external etc?
3. Do you agree that one cause of stress is worry over your health?
4. Do you agree that if that worry over your health was removed then ceteris paribus, your overall stress would decrease?
5. Do you agree that a reduction in stress would reduce your risk of CVD?
6. Do you agree that if the doctor gave you a pill and convinced you that this would reduce your risk of CVD then UNLESS the pill also caused you stress, then your stress would reduce and therefore CVD risk would lessen?
7. Therefore blogs that say statins are risky, don’t work etc etc make it less likely you’ll believe. BUT remove the blogs, let GPs prescribe a placebo (thus no side effects) convince us it will do us good and…it will.
This would be called a fully formulated straw man argument. Carefully define the terms of any discussion, then the logic follows. It would be better set up by starting, ‘You MUST agree that stress is a major cause of heart disease’. That removes the possibility of any disagreement right up front. However, I would change the terms of the discussion to the following. Do you think it is terrible that pharmaceutical companies distort and manipulate clinical trial results? The steps that would then follow your, unspoken but assumed, agreement (with my clearly sensible statement) would end up in a very different place. I do love logic, but it is a terribly tricky thing.
The fruit “asam keping” contains citric acid, tartaric acid, malic acid and ascorbic acid, hydroxycitric acid, and flavonoids.[2]
Science Daily:
The fruit of the ‘asam keping’ tree can be used to prevent atherosclerosis — that is the hardening and narrowing of the arteries -, according to research.
Dr Suraya A. Sani, recent PhD graduate from The University of Nottingham Malaysia Campus (UNMC), has been working with a tropical fruit, locally called asam keping, under the supervision of Dr Teng-Jin Khoo at UNMC’s School of Pharmacy.
Funded by the Sarawak Tunku Abdul Rahman Scholarship, she was able to spend her time on research work for the first two years at UNMC and a year working on her research at the Centre for BioMolecular Sciences at University Park, The University of Nottingham, UK under the co-supervision of Professor Dr Jonas Emsley.
Dr Suraya A. Sani conducts research on the medicinal properties of the Garcinia plant species; a plant species which is largely available in Malaysia and throughout Southeast Asia. The purple mangosteen tree and asam keping is from the Garcinia species.
Dr Suraya’s research led her to the findings of the medicinal role of specific plant secondary metabolites that exist in the Garcinia species, which is found in Malaysia in abundance. The fruit of the asam keping tree can be used to prevent atherosclerosis, the hardening and narrowing of the arteries.
full article here: https://www.sciencedaily.com/releases/2016/09/160905130249.htm
I don’t think exercise is only about calories expended. It also increases metabolism. Of course, if you make up for it with lots of bad food, you won’t be lean. You see guys who have laborious jobs and big fat bellies all the time.
Also, I have not ignored the point of this article, which is stress, at all. I have been thinking very hard about it and am trying to make changes. I was doing well, too, until a couple of things happened yesterday and today and I am afraid that my resolutions are failing…It seems as I get older I have more trouble with anxiety and worry.
Foraging. There are a number of greens that grow wild but I have not learned them although I have been shown a time or two. I’ve got a great book with incredible pictures. Turns out the lilies in our little pond have edible roots but I’m not sure I want to sacrifice them. In the book was wild carrot which I readily found but the so-called carrots are small and hard. There are wild walnuts that grow here although learning to shell them is on my “do” list, many people here know how. They are black walnuts rather than English, a slightly different taste. We have found a couple of species of wild mushroom. One grows quite copiously and we have dried them and have a few bags in the freezer. There are hawthorn trees which would be more of an herb. Right now I am waiting for the paw-paws to ripen. A delectable, custard-like fruit. I have made a year’s supply of jam from wild blackberries and raspberries. Of course, I don’t eat too much of that now. There are also wild elderberry bushes, but that again is more for medicinal purposes, supposedly antiviral. We eat venison, too. There’s a little fruit that grows close to the ground called a May apple.
Two papers that may be of interest,
Ceriello et al. Cardiovasc Diabetol (2016) 15:123 DOI 10.1186/s12933-016-0440-3
Glucagon and heart in type 2 diabetes: new perspectives
and J Clin Hypertens (Greenwich). 2014;16:524–529.
Acute Effects of an Oral Nitric Oxide Supplement on Blood Pressure, Endothelial Function, and Vascular Compliance in Hypertensive Patients (Comment: a natural solution to blood pressure)
Not bright enough to read and understand this. What type of Oral Nitric Oxide Supplement do you need to take to reduce BP
l-arginine plus l-citrulline
Tried those and they didn’t work.
Then your problem is not a lack of NO, unless you are taking something else that interferes with NO synthesis. You may also wish to look for more unusual causes of raised BP, such as sub-clinical Conn’s syndrome. Found to be a cause in around 15% of people – if the doctor actually looks for it.
Dr. Kendrick,
Practical questions:
L-arginine dose. One 500 mg pill, or a 6 gram scoop of powder?
L-citrulline dose. One 750 mg pill, or a 3 gram scoop of powder?
Those seem to be the available ranges. What’s to little; too much??
These are amino acids. Must they be taken alone to avoid their disappearance into a protein melange with a meal?
Mikecawdery: if this has been answered before, I apologize… How do I search for papers you mention? Can you outline the steps?
Thank you.
It seems that there is an oral NO supplement on the market in the form of a lozenge to be sucked and this study shows both a reduced SBP and a relaxing of blood vessels. The BP reduction was around 5mm Hg as i remember which I suspect is of limited clinical benefit.
Witn regard to L-arginiine (100mg capsule) since taking it I have had to reduce the dose rates of my antihypertensive drugs to prevent my SBP going beliow 90 mm Hg. This does not mean it will work for any one else; it may be worth trying it but no guarantees
Sorry 500mg capsule
Mike
There is of course beetroot and garlic, which were even appoved of in “Trust me, I’m a doctor”
I take beetroot occasionally and it does lower my BP
If one wishes to get of BP meds what is the best way to go about it. What can I expect if I stop taking them and how long before my body gets back to normal.
http://medstopper.com
Search for the drugly there.
Be patient, go slowly, expect rebound effect.
Thanks for that. Would you expect blood pressure to go up until your body gets used to going without the meds.
If the root cause of the hypertension is still unresolved, then it will go up. This should be obvious. The big Question is by how much and how fast.
This is not something to be done without self monitoring closely.
One has to make up one’s mind as to what is acceptable as an upper limit of BP, e.g. 140/90, sitting comfortably, having rested for 10 minutes.
It would be very wise to plot BP values on a sheet of paper or with a spreadsheet software. This would show where things are going (trend + variations vs. time of day…) & may even allow adjustments to the timing of meds.
Be scientific about it, measure multiple times a day. Data, data, data. Let the numbers be the guide.
For majority of HBP cases the cause is unknown. That’s why the medical profession creatively calls it “essential hypertension”. Thus, if there’s a rebound in BP after discontinuing the meds, it’s not because the root cause is unresolved but because you removed a pharmacological agent that was lowering it. For a great discussion on HBP and at what levels it needs lowering, look up “Malignant Medical Myths”.
I am taking losartan and felodipine. Are these ok to cut yourself with a tablet cutter.
We never cared about BP but both me an my wife have now noticed that a strict LCHF living not only amazingly improved our general state of health but for both of us we now, at 70, and for several years, register the blood pressures 110/60 at rest. Though it does not seem to impress on my cardiologist.
They can be quite special, just like Endos.
Mr. Chris
Corruption is of course a major problem. There is, as you are aware, a revolving door between US government agencies, the medical research establishment and Big Pharma. This can and does result in “odd” consequences. But in general money and status has displaced integrity and truth across the board; there is unlikely to be a satisfactory resolution to this problem.
Hypertension.
A while back Dr Kendrick wrote “Potassium, Your Invisible Friend” on this blog. One of the various benefits cited is the lowering of blood pressure.
This research article might explain its workings.
http://hyper.ahajournals.org/content/68/4/904.abstract?etoc
It’s hard to tell though, with all the acronyms, jargon, and strange syntax.
There’s no GoogleTranslate for this stuff.
Anybody?
Is there anyone here who is anti-statins? If so then I strongly suggest you contact the writer of this article as it is being widely publicised to reassure the public (they must be reading my posts) and in fact stress is being created in those who do NOT take statins as they may now be worried their chances of a heart attack have increased
https://www.theguardian.com/society/2016/sep/08/statins-prevent-80000-heart-attacks-and-strokes-a-year-in-uk-study-finds
Maybe Dr Kendrick should write a response…in the Guardian
I stopped taking statins in March 2015 in spite of the immense pressure put on me by my gp, consultants, nurses and Uncle Tom Cobblely. What the piece in the Guardian doesn’t tell you that the statistics upon which this incredible number is based, come from the corporations that make the damn stuff! In fact the source of the data doesn’t get a mention.
Six months after I had my heart attack (in 2012), the consultant in charge of my case told me, when asked, that I had a 50% chance of another heart attack. This in spite of the fact that at the time, I was on Atorvastatin which had reduced my total CH down to about 1 and left me feeling awful. How does that square with the figures cited in the study? or in the one I mentioned earlier which talked of a 1/3rd reduction in heart attacks (or is that deaths, it’s not clear).
Here’s the full statins study http://www.thelancet.com/journals/lancet/article/PIIS0140-6736(16)31357-5/fulltext
More on mindfulness.
It seems that mindfulness can make fibromyalgia patient think they feel better, but does nothing to effect underlying autonomic control.
What does this say about stress and strain management?
http://www.ncbi.nlm.nih.gov/pubmed/27518489?dopt=Abstract
F.A.O. Gay Corran’s entry dated 21 Aug.
I keep revisiting these blogs and many of the symptoms of your family member seem to be the same as mine now e.g. bruising and esp. stress/panic attacks, which I’m now getting.
You seem to have got excellent results from vitamins such as C and D, and also niacin.
Would you mind providing some further details? Such as:
How did you put a “regime” together, after reading Pauling and others?
What sort of quantities of vit C and so on?
How long did it take for improvements?
Kind regards
With Dr Kendrick’s permission, if given, please read the article I wrote a while ago, (below) on what helped a member of my family who was in a state of utter desperation following years of unbearable bullying in a marriage he was finally able to leave. We bought the books I recommend in the article, and following the advice in them led to complete recovery and the resumption of a normal happy and useful life.
Another Way Out of Addiction
Whenever I hear of tragedies like Robin Williams’ suicide, I want to reach out to every alcohol and drug addict with one of Dr Abram Hoffer’s books in my hand. It astonishes me that the Twelve Steps programme and its variations is still the mainstream method recommended for people who are crying out for help with addiction.
The themes of self-blame, abasement, atonement by the relapsing addicts for the wrongs done to those who love them, seem to me to be incompatible with helping people whose self-esteem is already below rock bottom.
No one wants to be an addict. Those who remain abstinent or clean by heroic will power and cognitive behavioural therapy group support systems almost always fight a daily battle with their desperate need. They almost inevitably suffer depression so appalling that many live half-lives sunk in black despair, or succumb as Robin Williams so tragically did.
The co-founder of AA tells the story of depression following abstinence and how he found its cure with Dr Hoffer’s help. He tried to incorporate his good news into the AA method of helping alcoholics and was banned from the organisation he helped found. Told, in effect, to get lost.
Similar organisations refuse to allow anyone who has benefitted from this knowledge of how to cure addiction to inform their fellow group participants about it. In one group the salaried leader said she would be out of a job were it not for “you guys”, the people who relapse and need the support of the group she ran.
According to Dr Abrams and his co-authors, when the stress centres are damaged, when the neurotransmitters misfire, when the adrenaline and fight or flight hormones are in constant play with no let up, the addict has no choice but to seek relief from what becomes unendurable need.
It’s a physiological issue; indeed, a biochemical, metabolic one, if you like. It’s amazing how soon the psychological problem disappears when the sufferer sorts the deficiency problem of nutrients needed for normal nerve function.
Stress, especially prolonged and unremitting stress, and alcohol/drug use deplete the nutrients needed for neurological functioning. Alcoholics are always severely deficient in essential vitamins and minerals, as are drug addicts. Replace those and normal function resumes. Lose them again and addiction once more takes over. By this same working, Post Traumatic Stress Disorder, however caused, will be helped by Dr Abrams’ nutrient regime.
Alcoholism is primarily a metabolic disease, rather than a psychological one. It is not caused by a character defect, and blame and shame have no place in this recovery programme.
This is explained in Dr Abram Hoffer’s book The Vitamin Cure for Alcoholism, and various other books by him. Joan Mathews Larson’s book Seven Weeks to Sobriety, (the Proven Program to Fight Alcoholism Through Nutrition), and The New Alcoholism Story Everyone Needs to Know, by Suka Chapel-Horst also explain how to cure addiction by putting the neurological system back into full operation, using nutrients rather than drugs.
Niacin (Vitamin B3 or Niacinamide) is the foundation of the course of nutrients needed, in much larger quantities than the usual RDA. All the B vitamins, along with C and D are also needed, along with magnesium and other trace elements and minerals. It is not true that large quantities of vitamins are dangerous: no one has ever died from a vitamin overdose.
Read the books; please read the books! All is explained, and you don’t need a prescription, though talking to a doctor sympathetic to giving it a go is certainly a good thing to do. Most doctors are geared up to prescribing drugs rather than vitamins, however, so you might need to be prepared to face scepticism.
This is not quackery. Or if it is, then it’s quackery that works: way to go!
The success rate is 75% in the first year, and rises as the years go by provided that the nutrient regime is continued, albeit in lesser quantities than needed during the first year.
This is in direct contrast to the relapse rate in AA and similar therapies, which is known to be 75% in the first year, and 95% in five years. This inevitably means that anyone mandated by the courts, social services or their doctors to undergo such therapy will be forever labelled as a hopeless addict, bound to relapse, as the statistics for failure in people attending such courses are well known.
If this post reaches just one person who wants to be free of addiction, who is prepared to read Dr Hoffer’s book and give his recommendations a go, then it was worth reaching out to you, or to someone who loves you enough to persuade you to try it.
Results are immediate: one notices a difference quite literally overnight. It’s cheaper than alcohol, or drugs. There is nothing to lose but addiction. There is everything to gain: health, joy; life itself.
Gay
Kind thanks for your swift, long and informative reply – I’m getting a copy of Hoffer’s book and it’s good to know it should be applicable to stress/anxiety/depression.
After reading your posts it seems you need all the self help you can get, so I very much hope Dr Hoffer’s book will point the way for recovery and your future well being. My very best wishes to you.
The THINCS website really is in need of updating. So much has happened, so much more information, books, youtube links, etc, since 2014. 2014!
Surely something should happen to what could be a valuable resource, but actually isn’t very much.
Keep up the good work.
I agree that the THINCS website needs updating. Or maybe it should be transferred to Dr K’s blog?
Dr Kendricks, I’m confused. On p. 191 of your book, ‘The Great Cholesterol Con’, you say:
Exactly! I’m on the same page and have stated the same on this blog and to date have not seen a response.
William:
Well on rereading the relevant parts, I think it’s pretty obvious that the Dr is protecting himself, after all there’s millions (if not billions) at stake here. I can only go by my own experience as a patient but when I challenged the statin orthodoxy over 18 months ago, I was put through the proverbial mill at a cost to the NHS (that’s us) of most likely thousands of pounds, until they finally ‘gave up’ on me. This ain’t about health or medicine, it’s political economy.
So okay, I get an ‘extra two days of life’ if (and it’s a big if) I take a statin but that two days stuff is absolute rubbish (and then I get hit by a bus?).
How the hell do you calculate that? On paper (or computer) it probably makes some kind of a statistical ‘truth’ but not in the real world I live in. It echoes the comment I got from the ‘specialist lipid nurse’ I was sent to see, who also told me I’d live longer if I took statins but when I asked her how much longer, the conversation ended. It’s embarrassing to see otherwise (I assume) intelligent people effectively take a ‘flat Earth’ approach to ‘evidence’.
Stress
In 2008, 4 years before my heart attack, I discovered (by accident actually) that I had an under-active thyroid and was put on Thyroxine.
Within a day of taking the hormone, whilst out walking, I started to get terrible pains in my legs. When I queried my GP at the time, whether there was a connection between the Thyroxine and the leg pain, I was told there wasn’t one. So I got tested and I was told that I had ‘intermittant claudication’ or atherioschlerosis. Yet before the Thyroxine, unless I was climbing a mountain, I didn’t suffer pain whilst out walking.
So I must have had it for some time. So why did it start up after the Thyroxine but not before?
I need to put this in perspective. Since returning to the UK in 2002 I had been under extreme stress, like I’d never suffered before. I couldn’t get a job in spite of a lifetime of experience in the media, journalism and the arts, I was ‘too old’.
I spent over three years trying to get a job but eventually gave up as it was obvious what was happening. I’d get shortlisted over and over again, but never get the job. I was too old. Very depressing and very stressful. I kinda gave up, I was beaten.
Then in 2012 I had my heart attack.
I note in Dr Kendricks book ‘The Great Cholesterol con’, that when it comes to discussing stress, the doctor refers to the HPA Axis, Hypothalmic-Pituitary-Adrenal Axis, which is of course directly connected to the Thyroid.
Did my thyroid go wonky because of stress and this in turn upset the other feedback mechanisms (the HPA-Axis) or perhaps it was the other way around (the HPA Axis buggered my Thyroid)? Again, I queried my then GP about the connection between the heart and the thyroid (eg could it raise cholesterol levels?). He told me that “stress has nothing to do with my wonky thyroid”, nor could it raise cholesterol levels. I know he was wrong on at least the connection with raised cholesterol and when I questioned the consultant I was sent to see last year, I asked him the same questions, and got the same answers. There’s no connection between stress and either the heart or the thyroid, perhaps as Dr Kendricks points out, it’s just too damn difficult to measure and probably even more importantly, so would be developing a pill for it (unless it it’s called Revolution!)
Brilliant Dr Kendricks! Stress, it all makes complete sense. The other factors, for example, smoking, merely exacerbate an existing condition.
But beyond that, I can look at my own experience and of others in my family who died of heart attacks, among them my father and two of his brothers. My father was full-time trade union organiser for the Musicians Union and before that worked as a musician and an engineer. A talented guy, who died when only 47 and like his two brothers who died of heart attacks, lived I venture, a stressful existence (they were all Communists and very active from the 1930s onwards).
And interestingly, my return to the UK after 30 years abroad, was not voluntary, so I returned to a country I barely knew (I was born in London and lived there the first 30 years of my life), with family gone, friends moved, died. Not a pleasant experience for me. Talk about social-dislocation!
Then add in the fact that in spite of all my skills and experience, I was surplus to requirement here, is it any wonder I got sick? In fact, back then a friend who knew me before and after the move, was amazed at how well I was coping and told me so. Appearances are obviously deceptive. But I was/am depressed by my situation.
I might add, that I wasn’t overweight, I had a decent diet, my only sin was smoking but clearly that was enough to push me over the edge as it were.
Stress as a source of (mental) illness is after all a well established fact, so why not for heart disease? And stress as a cause explains virtually all the apparently contradictory ‘evidence’ that uses cholesterol to explain the condition.
What’s really sick about it is the fact that vested economic interests have prevented the truth from emerging. It’s the same with our diet. I read recently that all the research conducted on the effects of sugar on health was paid for by the sugar industry, who managed to shift the blame onto fat by fixing the findings!
So thank you Dr Kendricks!
I’ve read Dr Gabor Maté book – When the body says no – And i think its a wonderful book, it sheds, in my opinion, light on what stress ( or adrenals fatigue ) can do to human beings and what are the sources of stress. He talks about the HPA axis, and so does Hans Selye https://en.wikipedia.org/wiki/Hans_Selye
http://drgabormate.com/book/when-the-body-says-no/
have fun reading it, its well worth it.
Thanks for that. I’ll check it out on Abe books.
Whilst I have come in a bit late to this conversation, I would say – look a bit closer at Magnesium.
Stress – or strain if you prefer – depletes magnesium faster than a bullet train. Without enough of this essential electrolyte, which is a natural relaxant, many processes do not work properly, or do not work at all.
Diabetics are known to lose magnesium at a faster rate than non-Diabetics. SLE patients have been found to have low RBC magnesium.
The body will always try to keep equilibrium in the blood. To do that, it will pull nutrients from the cells. That is why plasma blood tests will rarely show deficiency states. Only when the cellular supply is exhausted will the blood level start to drop. As far as I understand, a normal blood test will not show true cellular deficiency.
It does not matter what the diet is if the body is losing nutrients faster than it can receive them. Of course, certain dietary factors like sugar and processed carbs, gluten, etc., will put added strain on the body because of their nutritional deficit and the body having to draw on its own resources to make up the missing elements and complete the digestive process, but it is the cumulative effects of stresses/strains that can trigger CVD.
Interestingly, when my own hub suffered a MI in 2012, the stress of it wiped my own magnesium reserves – and I was taking at least 400mg Mg every day! I have long suspected that giving him Mg may well have helped, but I wasn’t as informed back then (apparently, according to Dr. Robert Morse, a teaspoon of cayenne pepper in some water can stop a heart attack too – although quite how, I haven’t a clue. There must be something in it the body needs. I didn’t know that at the time either)
I read somewhere that apparently in some states in the US, Magnesium is carried in the ambulances for this purpose……
Hello Ali,
I have long believed this. I was told that plasma levels were a good indication of intra cell levels of Mg, how else can you measure?
Also there is the question of which form mg citrate etc is the best absorbed?
Do you have any ideas on that?
Sorry I didn’t reply earlier. Your response only just popped up in my inbox….!
Serum levels will give a better indicator of cellular deficiency than plasma. Unfortunately, the NHS tends to favour plasma.
Some feel that Transdermal Mg Chloride is better absorbed than oral versions, but Mg Malate or Glycinate/Bisglycinate seem to be better absorbed orally than most.
So . .