In most diseases it is best to start at the beginning and work forwards. This should be the case with cardiovascular disease (CVD) too. However, for complex reasons I found myself starting at the end, and working backwards. The main reason for this is that I had to start with certainty. Yet, almost everywhere I looked there was mush. For example, the epidemiology of CVD.
Now you would think that there would be agreement about how many people actually die from CVD in different countries and at different times. Not a bit of it.
A researcher: ‘The French have a low rate of CVD.’
A N Other researcher: ‘Oh well the French, they don’t agree with the normal definitions, they don’t classify CVD properly. Who knows what the true rate may be?’
True? False? A bit true? Taking another example. I have looked at the figures from the US and, you know what. Not a single person died of Ischaemic Heart Disease before 1948. Amazing. What was protecting them? [Dying from IHD is what you would also call a heart attack, or MI]. What was protecting them was the fact that IHD did not exist in the US as a disease classification, before 1948.
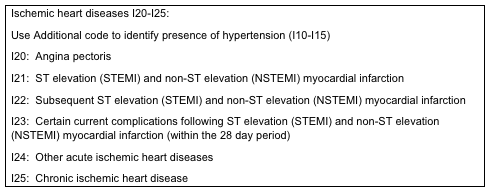
This then changed. In 1948 the World Health Organisation was created, and one of the first things they did was to create an International Disease Classification system (ICD). Heart disease is 1. Cancer is 2. (example for illustrative purposes only). Of course it is a bit more complex than that. Just to look in more detail at Ischaemic Heart Disease: [See box]:
Not every country took up the ICD system. Until 1968 the French did not use the ICD codes (so I am told, which no doubt means this is not true). Therefore, in France, statistics on deaths from IHD in France, before this date, are completely unreliable.
It goes without saying that, before 1948, no-one else used the ICD system either, because it did not exist. So, what can we tell about the epidemiology of CVD before 1948? Nothing. Or at least nothing you could hang your hat on. IHD would have been mixed within a much broader ‘Heart Disease’ in the death certificate statistics. And heart disease could mean almost anything, from cardiomyopathy to pericarditis, to atrial fibrillation.
Even after the ICD system was introduced, and even after France came on board, many countries clearly did not use it in the same way. Which is why the WHO set up the MONICA study.
‘The MONICA (Multinational MONItoring of trends and determinants in CArdiovascular disease) Project was established in the early 1980s in many Centres around the world to monitor trends in cardiovascular diseases, and to relate these to risk factor changes in the population over a ten year period. It was set up to explain the diverse trends in cardiovascular disease mortality which were observed from the 1970s onwards. There were total of 32 MONICA Collaborating Centres in 21 countries. The total population age 25-64 years monitored was ten million men and women. The ten year data collection was completed in the late 1990s, and the main results were published in the following years. The data are still being used for analysis.’
It was also an attempt to see if different countries were actually looking at the same diseases, and classifying them in the same way. Even after that, the data was still not absolutely clear cut, as further studies were then set up to see if the US system ARIC, and MONICA, actually matched each other. This was 1984.
‘To foster collaboration between the World Health Organization MONICA Project and the NHLBI Study of Atherosclerosis Risk in Communities (ARIC). To ensure that valid comparisons could made between findings in MONICA and ARIC by supporting activities to standardize coding, classification, and analysis of coronary and stroke events, risk factors, and medical care according to MONICA protocol.’
In simple terms, the US has its system, ARIC, and Europe had its system MONICA. Do they actually match? In short we can see that, even as late as 1984, there was clear uncertainty about how diagnoses were being made and how data were being gathered around the world. Did it all match, or not.
Given such uncertainly on both definition and diagnosis, can we say that the US epidemic of CVD in the 1960s actually happened. Or were doctors just putting IHD on death certificates when they didn’t really know what killed the patient. Personally, I think the epidemic did occur. Actually I think it happened a bit earlier. It is my belief that it took a while for US doctors to start using the new-fangled WHO ICD system.
Anyway, the point I am trying to make is that it is incredibly difficult to find the ‘bedrock.’ By which I mean facts that are inarguable. Things you can base your thinking on that are absolutely true, or that are as close to absolutely true, as possible.
Which is why I ended up at the end, the formation of the final, often fatal, blood clot. A blood clot which, generally, forms over an existing atherosclerotic plaque. There is widespread agreement that this is the case. So we can, I think safely, start here.
[There are, undoubtedly other things going on, such as sympathetic stress, mitochondrial damage and acidosis with heart muscle. that play a hugely important role. But the clot is, usually the final event
It is also widely agreed that factors which increase blood clot formation (thrombophilc factors) increase the risk of dying from CVD, and that things that reduce blood clotting reduce the rate of death from CVD. Here are a few things that increase the risk of blood clots forming, in no particular order:
- Dehydration
- Waking up in the morning/getting up in the morning
- Acute physical stress
- Acute psychological stress
- Having a high fibrinogen level
- Diabetes
- Cocaine use
- Smoking
- Cushing’s disease
Here are some of the things that reduce the risk of blood clots
- Haemophilia
- Von Willibrand Disease
- Aspirin
- Moderate alcohol consumption
- Clopidogrel
- Yoga
- Regular exercise
I suppose I should add that all of the things that increase the risk of blood clotting also increase the risk of death from CVD, and vice versa.
This is hardly a complete surprise. If blood clots kill you, things that reduce blood clots will prevent you from dying, and vice-versa. Let us not fall to the ground in stunned amazement over this statement of the bleeding obvious.
At this point, and slightly out of sequence, I would like to introduce statins to the list of factors that reduce the risk of blood clots
Readers of this blog know that I am not keen on statins, to say the least. However, if the studies are to be believed, they do reduce the risk of CVD. Not to any great extent, but the effect certainly does exist. Many people use this fact to attack my view that raised cholesterol does not cause CVD. ‘Well, what about statins,’ they bellow in delight. ‘They lower cholesterol and reduce the risk of CVD. Case proven…next’
Well, as with all drugs, statins do many other things than lower cholesterol levels. For example:
‘Recent studies have shown that statins reduce thrombosis via multiple pathways, including inhibiting platelet activation and reducing the pathologic expression of the procoagulant protein tissue factor.’1
So, as they say, there. In fact, one could quite sensibly propose that statins work pretty much the same as aspirin. They are anti-coagulants, and lowering blood cholesterol is simply a nasty and unfortunate side-effect of statins.
In reality, statins have a far more important effect on CVD (through other actions also related to clot formation) that I will get to later. I just thought I would pop that statin fact in. I even provided a reference. I have not really done much referencing in this series up to now. I believe that it is very simple to type, for example, ‘regular exercise and reduced thrombus formation’ into Google and see what you get. Or ‘Yoga and reduced blood coagulation.’
Where was I? Oh yes. Things that increase blood clot formation are more likely to kill you from CVD, and vice versa. Nothing controversial here. But the potentially controversial bit starts right here.
Are there two processes or one?
Currently, whilst conventional thinking on CVD accepts that blood clot formation is almost always the final event in CVD. This represents a completely separate process to the development of the atherosclerotic plaque itself. In short, we have two unrelated physiological processes:
- Plaque formation
- Clot formation on top of plaque
I apologize for saying, essentially, the same thing in different ways. But I think it is important.
Strange then, is it not, that plaque formation and clot formation share so many risk factors? Smoking, for example. Diabetes, for example. In fact, you could say (with certain provisos) that the risk factors for plaque formation and blood clot formation, are exactly the same.
Which gives one to think. Well it certainly gave me to think. Could it be that plaque formation, and blood clot formation, are simply two different manifestations of exactly the same underlying disease process. From a pure scientific perspective, I liked the idea. I liked it because it seems clumsy to have a disease, CVD, that is made up of two, essentially unelated processes
In medicine, as in all of science, one single disease process always looks much better, much cleaner, and much more likely to be right. This is the principle of Occam’s razor:
‘The principle in philosophy and science that assumptions introduced to explain a thing must not be multiplied beyond necessity, and hence the simplest of several hypotheses is always the best in accounting for unexplained facts.’
Next: The four step process of CVD
References:
1: http://www.ncbi.nlm.nih.gov/pubmed/24422578
